- Rare Disease News
- Resource Library
- Rare Disease Facts and Statistics
- NORD’s Rare Disease Database
- Rare Disease Video Library
- What It Means To Be Undiagnosed
- Find A Rare Disease Organization
- Stories That Inspire
- RareEdu ® – Online Learning Platform
- Rare Disease Day
- State Resource Center – Find Local Resources
- Publications On Rare Disease
- Getting Help & Support
- Managing Your Disease
- How NORD Can Help
- Speak To Someone at NORD
- Rare Disease Center Of Excellence
- Patient Assistance Programs
- Explore Clinical Trials
- Find A Patient Organization
- Caregiver Resources
- State Resource Center – Discover Local Resources
- Rare Diseases Defined
- Financial & Medical Assistance
- Call Center & Information Services
- Bringing Together Your Community
- NORD Member List
- Start a Rare Disease Organization
- Membership Program
- Becoming Research Ready
- Launching Registries & Natural History Studies
- Patient-Focused Drug Development
- Rare Disease Centers of Excellence
- Continuing Medical Education (CME)
- Corporate Council
- National Partnerships
- Global Parnerships
- Diversity, Equity & Inclusion
- List of Rare Diseases
- Gene Therapy for Rare Disease
- Find Clinical Trials & Research Studies
- Request for Proposals
- Research Grant Programs
- Data Standards for Rare Diseases
- Resources for Patients
- Find a Rare Disease Care Center
- IAMRARE ® Program Powered by NORD
- Rare Disease Cures Accelerator (RDCA-DAP)
- Add Your Expertise
- Today’s Policy Issues
- NORD’s Policy Statements
- Rare Disease Advisory Councils
- NORD State Report Card
- Join the Rare Action Network®
- Policy & Advocacy Taskforce
- Contact your Representative
- Take Action on Key Issues
- Learn about our current policy goals
- Do-It-Yourself NORD Fundraiser
- Students for Rare
- Sports & Fitness Fundraisers
- Media Inquiries
- Attend An Upcoming Event
- Find a Rare Disease Patient Organization
- Stay Informed With NORD’s Email Newsletter
- Rare Disease Day®
- Share Your Story
- Careers At NORD
- Intern At NORD
- Jobs At Patient Disease Organizations
- Donate to NORD
- Volunteer with NORD
- Visit the NORD Store
- For Clinicians & Researchers
- For Patient Organizations

Rare Disease Database
Disease overview, signs & symptoms.
- Affected Populations
Disorders with Similar Symptoms
Standard therapies, clinical trials and studies, programs & resources.
- Complete Report

Wandering Spleen
Last updated: February 11, 2008 Years published: 1994, 2003, 2008
Congenital wandering spleen is a very rare, randomly distributed birth defect characterized by the absence or weakness of one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. The disorder is not genetic in origin. Instead of ligaments, the spleen is attached by a stalk-like tissue supplied with blood vessels (vascular pedicle). If the pedicle is twisted in the course of the movement of the spleen, the blood supply may be interrupted or blocked (ischemia) to the point of severe damage to the blood vessels (infarction). Because there is little or nothing to hold it in place the spleen “wanders” in the lower abdomen or pelvis where it may be mistaken for an unidentified abdominal mass.
The spleen is a small organ located in the upper left portion of the abdomen. The spleen removes or filters out unnecessary or foreign material, breaks down and eliminates worn out blood cells, and produces white blood cells, which aid the body in fighting infection. Symptoms of wandering spleen are typically those associated with an abnormally large size of the spleen (splenomegaly) or the unusual position of the spleen in the abdomen. Enlargement is most often the result of twisting (torsion) of the splenic arteries and veins or, in some cases, the formation of a blood clot (infarct) in the spleen.
“Acquired” wandering spleen may occur during adulthood due to injuries or other underlying conditions that may weaken the ligaments that hold the spleen in its normal position (e.g., connective tissue disease or pregnancy).
- Print / Download as PDF
- Next section >
- < Previous section
- Displaced Spleen
- Drifting Spleen
- Floating Spleen
- Pelvic Spleen
- Splenic Ptosis
- Splenoptosis
- Systopic Spleen
Some children with wandering spleen may have no symptoms (asymptomatic), while others may experience acute or chronic abdominal pain. In most cases, episodes of pain may be related to the spontaneous twisting and untwisting of the mobile spleen (torsion and detorsion) or of the blood vessels serving the spleen. Infants with wandering spleen may attempt to relieve pain by stretching. Other symptoms may include a bulging abdominal mass, constipation, bloating, nausea, vomiting, frequent difficult urination, and/or menstrual problems in women.
In some cases, the spleen may lack proper blood supply due to the twisting of the splenic arteries. In these cases, symptoms may include abdominal pain, abnormal enlargement of the spleen (splenomegaly), bleeding into the abdomen (infarct), the accumulation of fibrous tissue in the spleen (fibrosis), and/or decay of splenic tissue (necrosis). In severe cases, blood flow into the spleen is diminished and the spleen may become greatly enlarged, as it accumulates (sequesters) blood elements such as platelets and red blood cells. Resulting symptoms may include fatigue, weakness, blood in the stools, anemia, bloody vomit (hematemesis), and/or an abnormally low level of blood platelets (thrombocytopenia).
In adulthood, wandering spleen most often causes abdominal pain or present as an abdominal mass that does not cause symptoms (asymptomatic).
The exact cause of wandering spleen is not known. Researchers suspect that multiple factors play a role in the development of the disorder (multifactorial).
Babies may be born with a wandering spleen that may be the result of a defect in a certain area of the developing embryo (mesogastrium dorsum). This is the area of the embryo that gives rise to the ligaments that normally hold the spleen in the upper left abdomen. Affected children may be missing one or all of these ligaments, or, if present, the ligaments are not positioned properly. Symptoms usually develop due to the abnormal position of the spleen in the lower abdomen or because of the abnormal enlargement of the spleen (splenomegaly).
Wandering spleen may occur during adulthood because of accident or injury, another underlying disorder (e.g., connective tissue disease), or the abnormal relaxation (laxity) of the ligaments caused by pregnancy.
Affected populations
Wandering spleen, whether it is a condition with which a baby is born (congenital form) or is the result of multiple births in women or some sort of accident that may affect men and women (acquired form), is an extremely rare disorder. Fewer than 500 cases of wandering spleen have been reported in the medical literature.
The incidence of wandering spleen is unknown and, because the condition may be underdiagnosed, is difficult to determine. It usually reported between the ages of 20 and 40 years with sex ratios of 7 females to 1 male. Most women are of reproductive age at the time of presentation. Children make up about a third of all cases, with 30 percent under 10 years of age. Among such children, the male-female ratio is 1:1.
As noted, acquired wandering spleen is acquired usually during adulthood, and it affects females many times more frequently than males. This is probably due to the relaxation (laxity) of the splenic ligaments during the childbearing years. Pregnancy is thought to contribute to the laxity, which increases the frequency of acquired wandering spleen among women who have had children.
Symptoms of the following disorders can be similar to those of wandering spleen. Comparisons may be useful for a differential diagnosis:
Peritonitis is a common disease characterized by the inflammation of the membrane that lines the abdominal wall (peritoneum). It may be caused by bacteria or other infectious organisms that enter the abdomen through a wound or hole (perforation) in one of the abdominal organs (e.g., ruptured appendix). Symptoms may include abdominal pain and rigidity, enlargement of the abdomen, vomiting, decreased bowel function, nausea, and/or an abnormally rapid heartbeat (tachycardia). If not treated, late symptoms may include chills, fever, rapid breathing, and/or shock.
Appendicitis is a common disease characterized by the acute inflammation of the appendix. If left untreated, the appendix may burst and cause peritonitis. The most common symptoms of appendicitis include pain in the lower right abdomen, vomiting, fever, and/or abdominal tenderness and rigidity. Treatment involves the prompt surgical removal of the appendix.
Diverticulitis is a common digestive disorder characterized by inflammation of one or more of the sacs (diverticula) that can form due to protrusion of the inner lining of the colon through its intestinal wall. The major symptom of diverticulitis is pain near the groin in the lower part of the abdomen. Other symptoms may include pain when urinating, constipation, diarrhea or other changes in bowel movements, fever, and/or rectal bleeding. (For more information on this disorder, choose “Diverticulitis” as your search term in the Rare Disease Database.)
Intestinal obstruction is a common condition characterized by the blockage of the intestines and a lack of intestinal motility. This results in the failure of waste (feces) to pass through intestines and be eliminated. The most common causes of intestinal obstruction are adhesions from previous surgery, impacted stools, a narrowing of the bowel because of an inflammatory bowel disease, and/or the presence of a tumor. Symptoms may include a swollen abdomen, severe abdominal pain, nausea and vomiting, and/or constipation.
Cholecystitis is a common disease characterized by inflammation of the gall bladder. This disease, which is usually caused by the presence of gallstones, can be acute or chronic. Symptoms may include ongoing or episodic severe abdominal pain, chills, nausea and vomiting, indigestion, heartburn, gassiness, fever, and/or pain in the chest, shoulder, and back. There may also be some discomfort after eating, an intolerance to fatty foods, and/or a yellowish discoloration of the skin. (For more information on this disorder, choose “Cholecystitis” as your search term in the Rare Disease Database.)
Other common diseases may also have symptoms that are similar to those of wandering spleen. These include pyelonephritis, hiatal hernia, hepatitis, gastric ulcer, gastroenteritis, and/or pancreatitis.
The following disorders may be associated with Wandering Spleen as secondary characteristics. Comparisons are not necessary for a differential diagnosis:
Thrombocytopenia is a condition characterized by abnormally low levels of platelets in the circulating blood. When the spleen becomes enlarged, platelets or other blood elements may be “captured” (sequestered) in the spleen. Symptoms of thrombocytopenia may include excessive bleeding, the tendency to bruise easily, nosebleeds, and/or abnormally heavy menstrual flow in women. If an enlarged spleen (splenomegaly)is not detected in the abdomen, then some people with wandering spleen may be misdiagnosed with other blood disorders that involve low circulating platelets (i.e., autoimmune thrombocytopenia purpura).
Prune belly syndrome is a rare congenital disorder characterized by underdevelopment of the abdominal muscles. The syndrome is associated with a number of intestinal and urogenital abnormalities. Often, the attachments of the muscles to the bones are present, but the muscles are small in size and thickness. Children with prune belly syndrome typically have abnormally large abdomens and the skin may appear loose or lax. The chest may also have a horizontal depression (Harrison groove) or may be very narrow (pigeon breast). Some children with pune belly syndrome may have wandering spleen because of the underdevelopment of the ligaments that normally anchor the spleen in the upper left abdomen. (For more information on this disorder, choose “Prune Belly” as your search term in the Rare Disease Database.)
Other conditions that have been associated with wandering spleen include the absence or abnormal enlargement of a kidney, infectious mononucleosis, malaria, sickle cell anemia, and Hodgkin’s disease. (For more information on these disorders, choose “Malaria,” “Sickle Cell,” and “Hodgkin” as your search terms in the Rare Disease Database or use “splenomegaly” as your search term to find other diseases that include an enlarged spleen.)
The diagnosis of wanderin. spleen is suspected when the pain associated with an abdominal mass can be relieved by moving it toward the upper left quadrant of the abdomen, the normal position of the spleen. Wandering spleen may be confirmed by specialized examinations such as ultrasonography and CT scan that enable the physician to view the structure, size, and placement of the spleen within the abdomen or pelvis. Specialized ultrasound tests (i.e., Doppler studies) may show impaired blood flow in and out of the spleen. Radioisotopic scanning (technetium 99 sulfur colloid scan), another imaging test, allows the physician to determine how well the liver and spleen are functioning. Low spleen function (functional asplenia) may suggest that the organ is damaged as a result of arterial obstruction (infarct).
The treatment of wandering spleen depends on the severity of symptoms and a thorough evaluation to determine the size, location, and functional status of the spleen. Since the spleen helps to maintain the proper function of the blood and immune system, most treatments are aimed at conserving the spleen and maximizing its function. However, since a person can live reasonably well without a spleen, surgical removal is considered.
The most conservative approach to the treatment of wandering spleen includes watchful waiting while observing splenic function and/or enlargement. Prevention of injury by avoiding contact sports or other activities that might threaten the spleen is also a part of the conservative approach.
For children with congenital wandering spleen who are experiencing episodes of torsion and acute pain, the treatment of choice may be surgery that anchors the spleen back in the proper position in the upper left abdomen (splenopexy). In many cases, the spleen can be preserved and the risk of torsion and infarct is reduced. Preservation of the spleen is preferred to removal through surgery because absence of the spleen can make a person vulnerable to certain infections.
If wandering spleen causes chronic abdominal pain, abnormal enlargement of the spleen, and/or deficiencies of one or more necessary blood elements (i.e., thrombocytopenic hypersplenism), the treatment of choice is usually surgery to remove the spleen (splenectomy). Acute abdominal pain associated with wandering spleen is considered a surgical emergency and may require immediate splenectomy.
The potential complications of complete removal of the spleen (splenectomy) may include postsplenectomy infection syndrome, which includes life-threatening bacterial infections (sepsis). People who have had a splenectomy are at higher lifetime risk for serious infections than the general population. Immunizations to boost immunity against haemophilus influenzae B, streptococcus pneumoniae, seisseria meningitis, and other contagious diseases are usually administered before the splenectomy is performed. All people who have had a splenectomy must be observed carefully in case of fever or other symptoms of infection. Antibiotics may be prescribed to help prevent infectious disease (prophylaxis), especially in children under the age of 2 years.
Information on current clinical trials is posted on the Internet at www.clinicaltrials.gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government website.
For information about clinical trials being conducted at the National Institutes of Health (NIH) Clinical Center in Bethesda, MD, contact the NIH Patient Recruitment Office:
Tollfree: (800) 411-1222
TTY: (866) 411-1010
Email: [email protected]
For information about clinical trials sponsored by private sources, contact:
www.centerwatch.com
REVIEW ARTICLES
Benevento A, Boni L, Dionigi G, et al. Emergency laparoscopic splenectomy for wandering pelvic spleen: case report and review of the literature on laparoscopic approach to splenic diseases. Surg Endosc. 2002;16:1364-65.
Satyadas T, Nasir N, Bradpiece HA. Wandering spleen: case report and literature review. J R Coll Surg Edinb. 2002;47:512-14.
Gayer G, Zissin R, Apter S, et al. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001;74:767-72.
Desai DC, Hebra A, Davidoff AM, et al. Wandering spleen: a challenging diagnosis. Douth Med J. 1997;90:439-43.
Horwitz JR, Black CT. Traumatic rupture of a wandering spleen in a child: case report and literature review. J Trauma. 1996;41:348-50.
JOURNAL ARTICLES
Upadhyaya P, St. Peter SD, Holcomb III GW. Laparoscopic splenoplexy and cystectomy for an enlarged wandering spleen and splenic cyst. J Pediatr Surg. 2007;42:E23-E27.
Schaarschmidt K, Lempe M, Kolberg-Schwerdt A, et al. The technique of laparoscopic retroperitoneal splenoplexy for symptomatic wandering spleen in childhood. J Pediatr Surg. 2005;40:575-7.
Brown CVR, Virgilio GR, Vazquez WD. Wandering spleen and its complications in children: a series and review of the literature. J Pediatr Surg. 2003;38:1676-79.
Kim SC, Kim DY, Kim IK. Avulsion of wandering spleen after traumatic torsion. J Pediatr Surg. 2003;38:622-23.
Steinberg R, Karmazyn B, Dlugy E, et al. Clinical presentation of wandering spleen. J Pediatr Surg. 2002;37:E30.
Andley M, Basu S, Chibber P, Internal herniation of wandering spleen/a rare cause of recurrent abdominal pain. Int Surg. 2000;85:322-24.
Peitgen K, Majetschak M, Walz MK. Laparoscopic splenopexy by peritoneal and omental pouch construction for intermittent splenic torsion (wandering spleen). Surg Endosc. 2001;15:413.
Nomura H, Haji S, Kuroda D, et al. Laparoscopic splenopexy for adult wandering spleen: sandwich method with two sheets of absorbable knitted mesh. Surg Laparosc Endosc Percutan Tech. 2000;10:332-34.
Danaci M, Belet U, Yalin T, et al. Power Doppler sonographic diagnosis of torsion in a wandering spleen. J Clin Ultrasound. 2000;28:246-48.
Vural M, Kacar S, Kosar U, et al. Symptomatic wandering accessory spleen in the pelvis: sonographic findings. J Clin Ultrasound. 1999;27:534-36.
Haj M, Bickel A, Weiss M, et al. Laparoscopic splenopexy of a wandering spleen. J Laparoendosc Adv Surg Tech A. 1999;9:357-60.
Kanthan R, Radhi JM. The ‘true’ splenic wanderer. Can J Gastroenterol. 1999;13:169-71.
Orphanet,the European database for rare diseases and contains a unique, multi-lingual nomenclature of rare diseases, along with several relevant resources.
Online Mendelian Inheritance in Man (OMIM) is a compendium of human genes and genetic phenotypes that is freely available, containing information on all known mendelian disorders and over 16,000 genes. Because OMIM is designed to be used primarily by physicians and other health professionals, although it is open to the public, the information is complex and users seeking information about a personal medical or genetic condition are advised to consult with a qualified physician for diagnosis and for answers to personal questions.
The information provided on this page is for informational purposes only. The National Organization for Rare Disorders (NORD) does not endorse the information presented. The content has been gathered in partnership with the MONDO Ontology. Please consult with a healthcare professional for medical advice and treatment.
- Assistance Programs
Patient Organizations
More information, rarecare ® assistance programs.
NORD strives to open new assistance programs as funding allows. If we don’t have a program for you now, please continue to check back with us.
Additional Assistance Programs
Medicalert assistance program.
NORD and MedicAlert Foundation have teamed up on a new program to provide protection to rare disease patients in emergency situations.
Rare Disease Educational Support Program
Ensuring that patients and caregivers are armed with the tools they need to live their best lives while managing their rare condition is a vital part of NORD’s mission.
Rare Caregiver Respite Program
This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder.
March of Dimes
Nih/national heart, lung and blood institute.
The information provided on this page is for informational purposes only. The National Organization for Rare Disorders (NORD) does not endorse the information presented. The content has been gathered in partnership with the MONDO Disease Ontology. Please consult with a healthcare professional for medical advice and treatment.
GARD Disease Summary
The Genetic and Rare Diseases Information Center (GARD) has information and resources for patients, caregivers, and families that may be helpful before and after diagnosis of this condition. GARD is a program of the National Center for Advancing Translational Sciences (NCATS), part of the National Institutes of Health (NIH).
- For Patients & Caregivers
- For Organizations

Every donation matters.
Your support helps to ensure everyone’s free access to NORD’s rare disease reports.

Torsion of a wandering spleen
Citation, doi, disclosures and case data.
At the time the case was submitted for publication Aliakbar Sahraei had no recorded disclosures.
Presentation
Acute abdominal pain.
Patient Data
- absence of the spleen in the left upper quadrant
- whirl sign: whirled appearance of hyperdense, nonenhancing splenic vessels
- enlarged spleen, without enhancement
Case Discussion
Wandering spleen is a rare condition in which the spleen migrates from its usual anatomical position, commonly to the lower abdomen or pelvis. Wandering spleen is rare, with a reported incidence of <0.5%.
It can present as an asymptomatic or painful abdominal mass, intermittent abdominal pain, or as an acute abdomen due to torsion 1,2 .
- 1.Lam Y, Yuen KK, Chong LC. Acute torsion of a wandering spleen. Hong Kong Med J. 2012;18 (2): 160-2. Pubmed citation
- 2.Raissaki M, Prassopoulos P, Daskalogiannaki M et-al. Acute abdomen due to torsion of wandering spleen: CT diagnosis. Eur Radiol. 1999;8 (8): 1409-12. Pubmed citation
1 article features images from this case
- Wandering spleen
16 public playlists include this case
- Spleen by frank fofie
- Long case by Gregory Makris
- FFR2B Long Cases_005 by David Ryan
- kejsy 17 by Lech Gradziński
- Abdomen - spleen by Edward Chan
- Spleen by K Hussain
- 6319 by Susheel K
- Kommische Fälle by Leivaditis
- hepatobilliary by simranjit bawa
- TESTS CASES by Farouq zeqlam
- Prüfung GI by Lisa Ruby
- viva 7/3 by Soumya Hareendranath
- GI 2 by Rahim Akram
- LIVER by Hala Elhadidi
- 1dom by Elias Sachawars ◉
- GI by Kenneth Kwok
Related Radiopaedia articles
- Splenomegaly
- Whirlpool sign (mesentery)
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Editorial Board

Advertisement
Torsion of wandering spleen: radiological findings
- Pictorial Essay
- Published: 18 May 2020
- Volume 27 , pages 555–560, ( 2020 )
Cite this article

- Mariano José Parada Blázquez ORCID: orcid.org/0000-0003-1248-9942 1 ,
- Daniel Rodríguez Vargas 2 ,
- Manuel García Ferrer 1 ,
- José Tinoco González 3 &
- Blanca Vargas Serrano 1
478 Accesses
8 Citations
Explore all metrics
Wandering spleen (or ectopic spleen) is a rare anomaly resulting from hyperlaxity or even absence of the ligaments that hold the spleen in its anatomical position. Although more frequently a congenital condition, it can also be acquired. Torsion of the vascular pedicle is its potential main complication with subsequent development of splenic infarct. In this paper we will describe the pathogenesis, clinical manifestations, treatment options and radiological findings which allow the diagnosis of this entity.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Torsion of the wandering spleen as an abdominal emergency: a case report

Splenic torsion mistaken for an ovarian cyst: a case report

Wandering spleen with volvulus of pancreas
Explore related subjects.
- Medical Imaging
Blouhos K, Boulas KA, Salpigktidis I, Barettas N, Hatzigeorgiadis A (2014) Ectopic spleen: an easily identifiable but commonly undiagnosed entity until manifestation of complications. Int J Surg Case Rep 5:451–454. https://doi.org/10.1016/j.ijscr.2014.05.010
Article PubMed PubMed Central Google Scholar
Rodriguez Vargas D, Parada Blazquez MJ, Vargas Serrano B (2019) Diagnóstico por imagen de anomalías en el número y localización del bazo. Radiologia 61:26–34. https://doi.org/10.1016/j.rx.2018.07.002
Article CAS PubMed Google Scholar
Ben Ely A, Zissin R, Copel L, Vasserman M, Hertz M, Gottlieb P, Gayer G (2006) The wandering spleen: CT findings and possible pitfalls in diagnosis. Clin Radiol 61:954–958. https://doi.org/10.1016/j.crad.2006.06.007
Priyadarshi RN, Anand U, Kumar B, Prakash V (2013) Torsion in wandering spleen: CT demonstration of whirl sign. Abdom Imaging 38:835–838. https://doi.org/10.1007/s00261-012-9944-9
Article PubMed Google Scholar
DeJohn L, Hal H, Winner L (2015) Wandering spleen: a rare diagnosis with variable presentation. Radiol Case Rep 3:229. https://doi.org/10.2484/rcr.v3i4.229
Zhang P, Dyer RB, Holbert BL (2018) A wandering spleen. Abdom Radiol (NY) 43:2525–2526. https://doi.org/10.1007/s00261-018-1488-1
Article Google Scholar
Viana C, Cristino H, Veiga C, Leão P (2018) Splenic torsion, a challenging diagnosis: case report and review of literature. Int J Surg Case Rep 44:212–216. https://doi.org/10.1016/j.ijscr.2018.02.032
Article CAS PubMed PubMed Central Google Scholar
Sojo Rodríguez V, Cañete Gómez J, Olivares C et al (2015) Acute abdomen due to torsion of the wandering spleen. Rev Esp Enferm Dig 107:229–230
PubMed Google Scholar
Castellón Pavón CJ, Valderrábano González S, Anchústegui Melgarejo P, Álvarez Álvarez J, Morales Artero S, Pérez Alzar C, Corrales Castillo S, Ramos-García Serrano F (2006) Esplenectomía laparoscópica por torsión de un bazo ectópico (wandering spleen). Cir Esp 80:406–408. https://doi.org/10.1016/S0009-739X(06)70996-4
Chawla S, Boal DK, Dillon PW, Grenko RT (2003) Splenic torsion. RadioGraphics 23:305–308. https://doi.org/10.1148/rg.232025110
Radillo L, Taddio A, Ghirardo S, Bramuzzo M, Pederiva F, Maschio M, Barbi E (2016) The great pretender: pediatric wandering spleen: two case reports and review of the literature. Pediatr Emerg Care 32:619–622. https://doi.org/10.1097/PEC.0000000000000642
Chauhan NS, Kumar S (2016) Torsion of a wandering spleen presenting as acute abdomen. Pol J Radiol 81:110–113
Aguirre Pascual E, Fontanilla T, Pérez Í, Muñoz B, Carmona MS, Minaya J (2016) Wandering spleen torsion-use of contrast-enhanced ultrasound. BJR Case Rep. 3:20150342. https://doi.org/10.1259/bjrcr.20150342
Lombardi R, Menchini L, Corneli T, Magistrelli A, Accinni A, Monti L, Toma P (2014) Wandering spleen in children: a report of 3 cases and a brief literature review underlining the importance of diagnostic imaging. Pediatr Radiol 44:279–288. https://doi.org/10.1007/s00247-013-2851-6
Reisner DC, Burgan MD (2018) Wandering spleen: an overview. Curr Probl Diagn Radiol 47:68–70. https://doi.org/10.1067/j.cpradiol.2017.02.007
Perez Fontan FJ, Soler R, Santos M, Facio I (2001) Accessory spleen torsion: US, CT and MR findings. Eur Radiol 11:509–512. https://doi.org/10.1007/s003300000547
Balci NC, Semelka RC, Noone TC, Ascher SM (1999) Acute and subacute liver-related hemorrhage: MRI findings. Magn Reson Imaging 17:207–211. https://doi.org/10.1016/S0730-725X(98)00154-4
Download references
Author information
Authors and affiliations.
Servicio de Radiodiagnóstico, Hospital Universitario Virgen del Rocío, Sevilla, Spain
Mariano José Parada Blázquez, Manuel García Ferrer & Blanca Vargas Serrano
Servicio de Radiodiagnóstico, Hospital Universitario Juan Ramón Jiménez, Huelva, Spain
Daniel Rodríguez Vargas
Servicio de Cirugía, Hospital Universitario Virgen del Rocío, Sevilla, Spain
José Tinoco González
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mariano José Parada Blázquez .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Parada Blázquez, M.J., Rodríguez Vargas, D., García Ferrer, M. et al. Torsion of wandering spleen: radiological findings. Emerg Radiol 27 , 555–560 (2020). https://doi.org/10.1007/s10140-020-01786-1
Download citation
Received : 02 April 2020
Accepted : 04 May 2020
Published : 18 May 2020
Issue Date : October 2020
DOI : https://doi.org/10.1007/s10140-020-01786-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Wandering spleen
- Vascular pedicle
- Find a journal
- Publish with us
- Track your research

Wandering Spleen
Wandering spleen can be found on imaging studies as a spleen that is located somewhere other than it’s usual position in the left upper abdomen. This article will discuss diagnosis, complications and treatment of wandering spleen.
What is Wandering Spleen?
A wandering spleen, also known as a floating spleen or splenoptosis, is a condition where the spleen migrates from its usual position in the upper left abdomen. The spleen is a crucial organ involved in filtering blood and fighting infections.
In individuals with a wandering spleen, the ligaments that hold the spleen in place are either elongated or weakened, allowing it to move freely within the abdomen. This mobility can lead to various health issues, including abdominal pain, bloating, and in severe cases, spleen torsion or infarction, where the blood supply to the spleen is cut off, leading to tissue death.
Symptoms of Wandering Spleen
The symptoms of a wandering spleen can vary widely from person to person. Some individuals may not experience any symptoms at all, while others may have noticeable signs. Common symptoms include:
– **Abdominal pain or discomfort:** Often reported in the lower abdomen and may vary in intensity. – **A palpable mass:** Some patients may feel a movable lump in their abdomen. – **Gastrointestinal symptoms:** Such as bloating, constipation, or indigestion.
In cases where the spleen becomes twisted (torsion), symptoms can quickly escalate to sharp abdominal pain, vomiting, and fever, necessitating immediate medical attention.

Causes and Risk Factors
The exact cause of a wandering spleen is not always clear, but it is often related to the weakening or malformation of the ligaments that secure the spleen. This condition can be congenital (present at birth) or acquired due to injury, pregnancy, or previous abdominal surgeries. Factors that may increase the risk of developing a wandering spleen include:
– **Ligamentous laxity:** Natural or acquired looseness of the ligaments. – **Trauma:** Abdominal injuries that may damage spleen ligaments. – **Pregnancy and childbirth:** Hormonal changes and physical strain can weaken abdominal structures.
Diagnosis of Wandering Spleen
Diagnosing a wandering spleen involves a combination of physical examinations, medical history, and imaging tests. Physicians may initially suspect the condition based on symptoms and a physical exam. Diagnostic imaging, such as ultrasound, CT scans, or MRI, plays a crucial role in confirming the diagnosis by visually locating the spleen’s position and assessing its condition.
Treatment Options
The treatment for a wandering spleen depends on the severity of the symptoms and the overall health of the patient. Options include:
– **Observation:** In asymptomatic cases, regular monitoring may be recommended. – **Surgical intervention:** For symptomatic patients, surgery is often necessary. The two main surgical options are: – **Splenopexy:** Reattaching the spleen to its correct position using synthetic materials or tissue. – **Splenectomy:** Removal of the spleen, typically reserved for cases where the spleen is damaged or has become necrotic.
Post-Treatment Care and Considerations
After treatment for a wandering spleen, patients will need to follow up with their healthcare provider for regular check-ups. If the spleen was removed, vaccinations against certain bacteria may be recommended since the spleen plays a critical role in fighting infections. Patients who undergo splenopexy should avoid activities that may risk abdominal trauma to prevent recurrence.
A wandering spleen is a rare condition that can lead to significant health issues if not properly addressed. Understanding the symptoms, causes, and available treatment options is important for anyone diagnosed with this condition. With timely and appropriate medical care, individuals with a wandering spleen can lead healthy and active lives. Always consult with a healthcare provider for an accurate diagnosis and personalized treatment plan tailored to your specific needs.
Similar Posts
Biliary dyskinesia.
Please read the disclaimer Biliary dyskinesia is a functional disorder of the gallbladder. This means that there is no blockage or anatomical problem of the gallbladder. Imaging of the gallbladder…
Fat Containing Ventral Hernia
Please read the disclaimer Ventral hernias are a common condition that occurs when an opening in the abdominal muscles allows abdominal tissues or organs to protrude. Among the various types…
Appendicolith Symptoms, Diagnosis, Imaging and Treatment
Please read the disclaimer Introduction: In this comprehensive guide, we will discuss appendicoliths, focusing on their symptoms, diagnosis, imaging methods, and available treatments. An appendicolith is a small, hardened piece…
Adrenal Nodule
Please read the disclaimer Adrenal nodules are abnormal growths or masses that develop in the adrenal glands, located on top of each kidney. These nodules often appear incidentally during imaging…
Papillary Renal Cell Carcinoma
Please read the disclaimer Papillary Renal Cell Carcinoma (PRCC) is a specific type of cancer that affects the kidneys. It is the second most common subtype of renal cell carcinoma…
IPMN Of The Pancreas (Intraductal Papillary Mucinous Neoplasm)
Please read the disclaimer Intraductal papillary mucinous tumor or IPMN is a cystic tumor that arises from the pancreatic duct. The pancreatic duct runs through the pancreas and carries digestive…
- Open access
- Published: 05 August 2013
Acute abdomen due to torsion of the wandering spleen in a patient with Marfan Syndrome
- Laura Leci-Tahiri 1 ,
- Afrim Tahiri 1 ,
- Rifat Bajrami 1 &
- Mehmet Maxhuni 1
World Journal of Emergency Surgery volume 8 , Article number: 30 ( 2013 ) Cite this article
7229 Accesses
7 Citations
Metrics details
Wandering spleen is a very rare defect characterized by the absence or weakness of one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. Patient symptomatology is variable and ranges from mere feeling of an abdominal lump to sudden abdominal pain due to infarction. Patients may have subacute to chronic abdominal or gastrointestinal complaints. Because of nonspecific symptoms, clinical diagnosis can be difficult; hence, imaging plays an important role. A major complication is splenic torsion, which is the cause of acute abdomen. We present a case of acute abdominal pain due to torsion of wandering spleen in a patient with Marfan Syndrome, valvular heart disease, and vertebral anomalies. Preoperative diagnosis was made on the basis of ultrasonography and computed tomography, which was later confirmed on surgery, and treated successfully.
Case presentation
A 36-year-old Albanian man presented to Emergency Unit with complaints of abdominal pain, two-week history of constipation, and a tumor in the right lower abdomen (Figure 1 ).

Tumor in the right lower abdomen.
The patient presented with features of Marfan syndrome: increased height, arachnodactyly, long limbs, contractures of the hand, pectus excavatum, genu recurvatum, and scoliosis. He had undergone mitral valve implantation 15 years previously, and had been treated with oral anticoagulants.
At admission, the patient was afebrile, pale, rundown, and fully conscious. His left lower extremity was oedematous under the knee. Abdomen was soft on palpation with a 20×9 cm mass palpable in the right hypogastric region.
Doppler examination of the lower extremity veins showed thrombosis of the left popliteal and left tibialis posterior vein. A vascular surgeon was consulted, and heparin with a high molecular weight, 7500 UI, was administered every 6 hours intravenously.
Due to lung problems, a pulmonologist was further consulted, who found pleuropneumonia in the left lung. The patient suffered from arterial hypertension and chronic cardiomyopathy.
Laboratory investigations showed mild anaemia and leucocytosis. Tumor markers were checked but were all within normal limits.
Ultrasound of the abdomen
Absence of the spleen in its normal position in the left hypochondrium, and presence of tumor mass in the right fossa inguinalis. Other organs of the abdomen were normal.
Magnetic resonance imaging of the abdomen and pelvis
Absence of the spleen in the normal location. The spleen was seen in the lower right hemiabdomen, enlarged, with the size of 18.7×8.5×20.8 mm and sacral meningocoele.
CT angiography of abdominal vessels
Splenic artery was divided by pancreatic artery, which was forwarded to the tail of pancreas giving it a “whorled appearance”, and from this level splenic vessels were thrombosed. Pancreas was moved forward without obvious radiological changes (Figures 2 and 3 ).
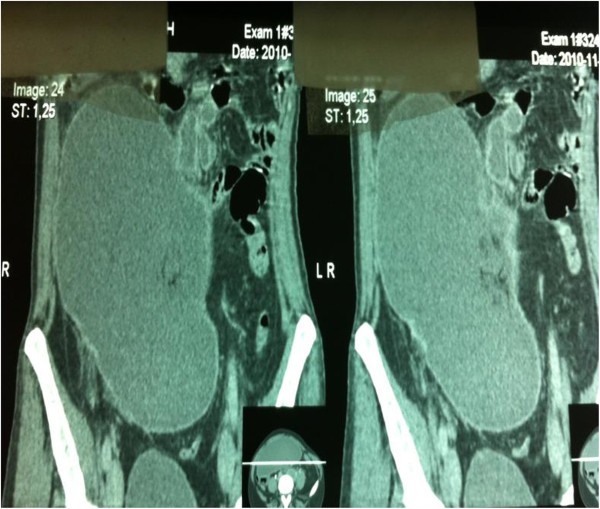
Anteroposterior Angio-CT showing enlarged spleen in lower right hemiabdomen.

Sagital Angio-CT showing size of spleen.
Operative findings revealed a huge spleen in the pelvic area with torsion of the vascular pedicle starting at the tail of the pancreas (Figure 4 ). The characteristic “whirl sign” can be seen in the area of the splenic vascular pedicle, indicative of torsion (Figure 5 ). Other internal organs were normal.
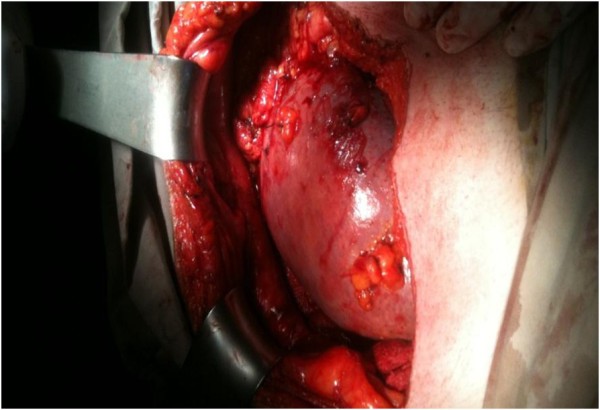
Huge spleen in right pelvic area.

“Whirl sign” in the area of the splenic vascular pedicle, indicative of torsion.
A total splenectomy was performed, as the organ appeared congested, it was likely infarcted and not likely to be salvageable (Figure 6 ).

Spleen with diffuse hemorrhagic and ischemic infarcts.
The patient recovered well after the operation. Antibiotics, analgesics, plasma, blood, low molecular weight heparin, vitamins and triple vaccination (against pneumococcus, hemophilus influenza, and meningococcus) were given.
He was discharged on oral anticoagulants because of heart disease.
Histology revealed acute thrombotic changes in arteries and veins of the splenic hilum, with diffuse hemorrhagic and ischaemic infarcts of the spleen.
Wandering spleen is an uncommon clinical entity, which rarely affects children and adolescents. Discussion in the literature has been limited to case reports and small case series [ 1 ]. The condition is not hereditary.
Congenital wandering spleen is a very rare randomly distributed birth defect characterized by the absence or weakness of one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. Instead of ligaments, the spleen is attached by a stalk-like tissue supplied with blood vessels (vascular pedicle). If the pedicle is twisted in the course of the movement of the spleen, the blood supply may be interrupted or blocked (ischaemia) to the point of severe damage to the blood vessels (infarction). Because there is little or nothing to hold it in place, the spleen “wanders” in the lower abdomen or pelvis where it may be mistaken for an unidentified abdominal mass.
“Acquired” wandering spleen may occur during adulthood due to injuries or other underlying conditions that may weaken the ligaments that hold the spleen in its normal position (connective tissue disease or multiparity) [ 2 , 3 ].
Van Horne, a Dutch physician, is credited with describing this condition in 1667 after performing an autopsy. In 1875, Martin, a German obstetrician, performed the first splenectomy for a wandering spleen [ 4 , 5 ]. Ten years later, splenopexy was described and considered superior to splenectomy, a differential preference that has changed several times over the years. Since Van Horne’s discovery, approximately 400 cases of wandering spleen have been reported worldwide. It is a rare entity accounting for less than 0.25% of splenectomies [ 6 ]. Twenty one cases of wandering spleen, including our present case, have been reported in the English literature during the past decade (Table 1 ). The majority of patients are female, in second and third decade of life. Computed tomography is the imaging method of choice for diagnosing wandering spleen. The usual location of wandering spleen is pelvis and left iliac fossae. We couldn’t find in literature the location in right iliac fossa, as our case showed. Abdominal pain, intestinal obstruction, nausea, vomiting, fever, and a lump in the abdomen or the pelvis are the common symptoms in all reported cases. Splenectomy is performed in most cases.
Discussion in the literature is limited, especially in cases with Marfan Syndrome and valvular heart disease. We have found only one case with wandering spleen in a child with Marfan Syndrome [ 7 ].
Marfan syndrome is caused by a defect, or mutation, in the gene that determines the structure of fibrillin-1, a protein that is an important part of connective tissue. It is an inherited disorder of the connective tissue that affects major organ systems of the body: the heart and circulatory system, thebones and muscles, and the eyes. A person with Marfan syndrome is born with the disorder, even though it may not be diagnosed until later in life [ 7 ].
As it is a generalized connective tissue disorder, congenital laxity of the primary ligamentous attachments of the spleen might predispose to splenic hypermobility and hence torsion in childhood, in contrast to the more common acquired form of splenic torsion seen in multiparous females that is believed to be caused by laxity of these ligaments owing to hormonal changes and multiparity [ 7 – 9 ].
Symptoms of wandering spleen are those typically associated with an abnormal size of the spleen (splenomegaly) or the unusual position of the spleen in the abdomen [ 9 , 10 ].
Patients maybe asymptomatic or may present with acute abdominal pain. The common clinical presentation is abdominal mass with pain. It may occur in people of all ages with a predilection for male under 10 years of age and for female patients in older age groups, being most common in multiparous women. Under the age of 10 the sex distribution is even, whereas over 10 years of age, females out number males by seven to one. A study involving 66 children under 10 years showed that 50% of wandering spleens were lost through acute ischaemia [ 7 , 9 , 11 ].
Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [ 6 , 12 , 13 ].
Splenopexy is the treatment of choice for a noninfarcted wandering spleen. One small case study in 2004 demonstrated successful laparoscopic splenopexy using a Vicryl mesh bag. Splenic preservation in cases of wandering spleen without rupture or infarction avoids the risk of overwhelming postsplenectomy sepsis, and a laparoscopic approach allows for shorter hospital length-of-stay and decreased postoperative pain [ 12 , 14 , 15 ].
Splenectomy should be done only when there is no evidence of splenic blood flow after detorsion of the spleen. In our patient, because of the intraoperative findings of splenic infarction, splenectomy was performed [ 12 , 16 ].
The possible diagnosis of wandering spleen should be kept in mind when CT shows the spleen to be absent from its usual position and a mass is found elsewhere in the abdomen or pelvis. Abdominal ultrasonography (with or without Doppler) and CT are useful investigative tools. Early intervention is necessary to reduce the risk of splenic infarction and other complications. An awareness of the condition together with the use of appropriate medical imaging can lead to the correct diagnosis.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Brown CV, Virgilio GR, Vazquez WD: Wandering spleen and its complications in children: a case series and review of the literature. J Pediatr Surg. 2003, 38: 1676-1679. 10.1016/S0022-3468(03)00582-7.
Article PubMed Google Scholar
March of Dimes Birth Defects. Internet: http://www.marchofdimes.com
Genetic and Rare Diseases. Internet: http://rarediseases.info.nih.gov
Dahiva N, Karthikeyan D, Vijav S, Kumar T, Vaid M: Wandering spleen: Unusual presentation and course of events. Abdom Imaging. 2002, 12: 359-362.
Google Scholar
Tan HH, Ooi LLPJ, Tan D, Tan CK: Recurrent abdominal pain in awoman with a wandering spleen. Singapore Med J Case Report. 2007, 48: 122-124.
Khoi L, Devan G, William WH, Darryl T: Splenic Torsion Requiring Splenectomy Six Years Following Laparoscopic Nissen Fundoplication. JSLS. 2012, 16: 184-188. 10.4293/108680812X13291597716861.
Article Google Scholar
Sodhi KS, Gupta P, Rao KLN, Marwaha RK, Khandelwal N: Marfanoid hypermobility syndrome and skeletal abnormalities in a rare case of torsion of wandering spleen. BJR. 2008, 81: 145-148. 10.1259/bjr/30123041.
Huai-Tzu ML, Kenneth KL: Wandering Spleen: An Unusual Association with Gastric Volvulus. AJR. 2007, 188: 328-330. 10.2214/AJR.05.0672.
Desai DC, Hebra A, Davidoff AM, Schnaufer L: Wandering spleen: a challenging diagnosis. South Med J. 1997, 90: 439-443. 10.1097/00007611-199704000-00017.
Article CAS PubMed Google Scholar
Befikadu S, Gudu W, Abseno N: Torsion of a pelvic wandering spleen as a cause of acute abdomen in a woman: a case report and review of the literature. Ethiop Med J. 2004, 42: 53-61.
PubMed Google Scholar
Fujiwara T, Takehara Y, Isoda H, Ichijo K, Tooyama N, Kodaira N, Kitanaka H, Asai T, Kawaguchi K: Torsion of the wandering spleen: CT and angiographic appearance. J Comput Assist Tomogr. 1995, 19: 84-86. 10.1097/00004728-199501000-00016.
Dawson JH, Roberts NG: Management of the wandering spleen. Aust NZJ Surg. 1994, 64: 441-444. 10.1111/j.1445-2197.1994.tb02249.x.
Article CAS Google Scholar
Romero JR, Barksdale EM: Wandering spleen: a rare cause of abdominal pain. Pediatr Emerg Care. 2003, 19: 412-414. 10.1097/01.pec.0000101582.65509.cc.
Khurana B: The Whirl Sign. Radiology. 2003, 226: 69-70.
Ben Ely A, Zissin R, Copel L, Vasserman M, Hertz M, Gottlieb P, Gayer G: The wandering spleen: CT findings and possible pitfalls in diagnosis. Clin Radiol. 2006, 61: 954-958. 10.1016/j.crad.2006.06.007.
Bakir B, etal: Acute torsion of a wandering spleen: imaging findings. Abdom Imaging. 2004, 29: 707-709. 10.1007/s00261-004-0174-7.
Download references
Author information
Authors and affiliations.
Clinic of Surgery, University Clinical Center of Kosova, Prishtina, Kosova
Laura Leci-Tahiri, Afrim Tahiri, Rifat Bajrami & Mehmet Maxhuni
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Afrim Tahiri .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
AT and RB performed the surgery, supervised the patient’s care, drafted the manuscript, and approved the version submitted for publication. LT and MM assisted with patient care and have been involved in drafting the manuscript. AT, LT and MM has been involved in drafting and revising the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Leci-Tahiri, L., Tahiri, A., Bajrami, R. et al. Acute abdomen due to torsion of the wandering spleen in a patient with Marfan Syndrome. World J Emerg Surg 8 , 30 (2013). https://doi.org/10.1186/1749-7922-8-30
Download citation
Received : 01 February 2013
Accepted : 23 July 2013
Published : 05 August 2013
DOI : https://doi.org/10.1186/1749-7922-8-30
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Marfan Syndrome
- Vascular Pedicle
- Acute Abdominal Pain
- Splenic Infarction
- Pectus Excavatum
World Journal of Emergency Surgery
ISSN: 1749-7922
- Submission enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Surg Case Rep
- v.119; 2024 Jun
- PMC11087991
Torsion of a wandering spleen in a pregnant patient presented with acute abdomen: A case report
Alemneh mitku chekol.
a St. Paul's Hospital Millennium Medical College (SPHMMC), Addis Ababa, Ethiopia
Aemro Tadesse Abzaw
b Tikur Anbesa Specialized Hospital (TASH), Addis Ababa, Ethiopia
Seyoum Hailu Abebe
Zelalem assefa semagn, barakad mohammed hassen, introduction and importance.
Wandering spleen may result in torsion or splenomegaly, which causes symptoms such as intestinal obstruction, nausea, vomiting, and swelling in the abdomen. There are few reports of wandering spleen torsion in pregnant mothers. The diagnosis and presentation of splenic torsion is variable and challenging during pregnancy. Herein, we present a case of torsion of a wandering spleen in a 30-year-old pregnant patient.
Case presentation
A 30-year-old female presented with a sudden onset of abdominal pain of three days' duration. There was lower abdominal mass and tenderness. Intraoperative findings revealed enlarged spleen located over the lower abdominal cavity with six times clockwise rotation of the splenic pedicle over itself. A splenectomy was performed. The patient was discharged on the 7th postoperative day and had an uneventful postoperative recovery.
Clinical discussion
Patient presentation could be asymptomatic, chronic left abdominal pain or symptoms and signs of complication. The most common complication of wandering spleen is torsion (Abell, n.d.). Splenic torsion is evidenced by mucosal bleeding, hematemesis, anemia or thrombocytopenia in our patient platelets level was 111,000 cells/μl which suggests vascular thrombosis. The other peculiarity during pregnancy is torsion of the spleen have higher mortality reaching up to 41 % (Lewis and Wolskel, 1962) which may be from delay in diagnosis or misdiagnosis.
There is high mortality associated with splenic torsion in pregnant patient reported in the literature. One of the explanations is misdiagnosis and delay in diagnosis of torsion of a wandering spleen in a pregnant patient.
- • Presentation of wandering spleen could be asymptomatic, chronic left abdominal pain, or symptoms and signs of complication.
- • The most common complication of wandering spleen is splenic torsion.
- • The diagnosis and presentation of splenic torsion are variable and challenging during pregnancy.
- • During pregnancy misdiagnosis for gynecologic emergencies leads to delay in management and associated poor outcome.
- • Clinicians should have high index of suspicion to avoid misdiagnosis and higher mortality reaching up to 41 %.
1. Introduction
Before Dietl's time there was a common understanding that a “wandering spleen” led women to experience hypochondria [ 3 ]. Wandering spleen is a rare condition that occurs when the spleen lacks one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. If a person is born with a wandering spleen that may be the result of a defect in a certain area of the developing embryo (mesogastrium dorsum) [ 4 , 5 ]. This is the area of the embryo that gives rise to the ligaments that normally hold the spleen in the upper left abdomen ( Fig. 1 ). Affected children may be missing one or all of these ligaments, or, if present, the ligaments are not positioned properly [ 6 ]. Acquired wandering spleen may occur during adulthood due to accident or injury, another underlying disorder (e.g., connective tissue disease), or the ligaments' abnormal relaxation (laxity) caused by pregnancy [ 4 , 5 ].

Normal anatomic position of the spleen with its relation with the pancreas, diaphragm, splenic flexure of the colon, stomach and kidneys. The ligaments run between this adjacent structures.
Symptoms of wandering spleen may include enlargement of the spleen (splenomegaly), abdominal pain, intestinal obstruction, gastric volvulus, nausea, vomiting, fever, and a lump in the abdomen or the pelvis. Some individuals with this condition do not have symptoms. The most common complication of wandering spleen is torsion and other complications are splenic infarction, splenic abscess, variceal hemorrhage, gastric volvulus, and pancreatic tail necrosis [ 4 , 5 , 7 ].
There are few reports of wandering spleen torsion in pregnant mothers [ 2 ]. The diagnosis and presentation of splenic torsion are variable and challenging during pregnancy. Although most of the cases presented as an acute emergency, in some instances, the attack lasts from several days to months, the patients having survived the acute onset with adherence of omentum and intestine [ 2 , 4 ]. There was a 41 % mortality when torsion occurred during pregnancy or the puerperium [ 1 ].
The diagnosis of wandering spleen is suspected when the pain associated with an abdominal mass can be relieved by moving it toward the upper left quadrant of the abdomen, the normal position of the spleen. Wandering spleen may be confirmed by specialized examinations such as ultrasonography and CT scans that enable the physician to view the structure, size, and placement of the spleen within the abdomen or pelvis. Specialized ultrasound tests (i.e., Doppler studies) may show impaired blood flow in and out of the spleen [ 4 ]. Because imaging procedures like CT scans are not routinely utilized during pregnancy due to possible radiation exposure, doctors rely on clinical data and ultrasonography when treating pregnant women who complain with acute abdominal pain. Due to operator dependence, ultrasonography may misdiagnose this type of situation while a pregnant woman is experiencing it [ 8 , 9 ].
The treatment of the wandering spleen depends on the severity of symptoms and a thorough evaluation to determine the size, location, and functional status of the spleen. The most conservative approach to the treatment of wandering spleen includes watchful waiting while observing splenic function and/or enlargement. Prevention of injury by avoiding contact sports or other activities that might threaten the spleen is also a part of the conservative approach. For children with congenital wandering spleen who are experiencing episodes of torsion and acute pain, the treatment of choice may be splenopexy. Preservation of the spleen is preferred for children than removing through surgery because the absence of the spleen can make children vulnerable to certain infections. If wandering spleen causes chronic abdominal pain, abnormal enlargement of the spleen, and/or deficiencies of platelets (thrombocytopenia, hypersplenism), the treatment of choice is usually surgery to remove the spleen (splenectomy) [ 10 , 11 ]. Acute abdominal pain associated with a wandering spleen is considered a surgical emergency and may require immediate splenectomy either through laparotomy or laparoscopy [ 10 , 12 ].
From literature reviews, there is no previously reported case of torsion of a wandering spleen in a pregnant patient from Ethiopia, and there are only a few cases reported in the rest of the world with high mortality as high as 41 %. Herein, we present a case of torsion of a wandering spleen in a 30-year-old pregnant patient. We wrote the case report following the SCARE criteria [ 13 ].
2. Case report
A 30-year-old female who was amenorrheic for 02 months with an unknown last normal menstruation period presented to the emergency department with a complaint of sudden onset of colicky abdominal pain of three days' duration which is over the left lower quadrant of the abdomen. She had associated frequent episodes of non-bilious non-projectile vomiting of ingested matter. There is no history of repeated treatment for malaria or chronic medical illness. She had no previous history of surgery. This is her fourth pregnancy with previous three live births.
At the time of the presentation, she was in pain. Her vital signs; blood pressure was 110/75 mmHg, pulse 104 beats per minute, temperature of 36.5 °C, and respiratory rate of 20 breaths per minute. Abdominal examination showed a distended abdomen, with deep and rebound tenderness over the right lower quadrant and left lower quadrant of the abdomen with a palpable smooth-surfaced mass over the lower quadrants of the abdomen. The rectum was empty with no blood or mass. The rest of the system physical examination was unremarkable.
Her investigations were remarkable on complete blood cell count (CBC) the platelet (PLT) level was 111,000 cells/μl and white blood cell count was 15,860 cells/μl with a neutrophil proportion of 85.6 %. Urine pregnancy test (UHCG) was determined and found to be positive. Abdominal Ultrasound showed a low-lying spleen located in the lower abdominopelvic cavity with no blood flow seen at the hilum. The spleen is homogeneously enlarged measuring 18.4 cm. The uterus is enlarged with singleton viable intrauterine pregnancy. Gestational age by biparietal diameter was 12 weeks plus 5 days.
After the patient was adequately resuscitated in the emergency department and produced adequate urine output, cross-matched blood was prepared, and the patient was taken to the operating theater for an emergency exploration. Intraoperative findings were 100 ml of serous fluid in the general peritoneum, and the enlarged blackish-colored spleen located over the right lower quadrant and left lower quadrant of the abdominal cavity ( Fig. 2 ). The spleen was rotated clockwise six times over its vascular pedicle ( Fig. 2 ) with accessory spleen over the splenic hilum ( Fig. 4 ). The spleen was wandering to the right of the midline and had no ligamentous attachments with the diaphragm and the posterolateral abdominal wall ( Fig. 3 ). The splenocolic and splenorenal ligaments were lax creating a long pedicle with a length of 8 cm measured from splenic hilum to pancreatic tail ( Fig. 3 ). After de rotation the spleen didn't regain its color No diaphragmatic defects or other abnormalities were identified ( Fig. 3 ). A splenectomy was performed.

An enlarged wandering spleen occupying the pelvis and lower quadrants of the abdomen. The splenic vascular pedicle was rotated clockwise around six times over itself.

Spleen taken out of abdominal cavity. A long splenic vascular pedicle after complete de-rotation of a six-time clockwise rotation of the spleen over its vascular pedicle. There are torturous and engorged veins over the lax gastro splenic and gastrocolic ligaments. Change in color of the spleen is not reverted after full de-rotation. Accessory spleen is located over the hilum of the spleen.

Accessory spleen located near the hilum of the spleen.
The postoperative course of the patient was smooth with sips started after 24 h. repeat CBC was determined on 3rd post-op day and the PLT level was 430,000 cells/μl and WBC was 12,800 cells/μl with a neutrophil proportion of 73.1 %. She took a 7-day course of antibiotics: ceftriaxone and metronidazole. On the seventh postoperative day, the patient was discharged with oral analgesics with 1 g of paracetamol per requirement. On top of that, the patient received health education on preventing post-splenectomy sepsis and was prescribed oral amoxicillin. On the fourteenth postoperative day, she was in better health and had healed wounds during her follow-up clinic visits. She received the polyvalent Pneumococcal vaccination and the conjugate Haemophilus influenza B vaccine during the third week following her operation; however, she was not immunized against Meningococcus and influenzas virus due to unavailability. The remainder of her visits, including the one on the thirtieth postoperative day, went well.
3. Discussion
Wandering spleen is a rare condition that occurs when the spleen lacks one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. The spleen is suspended in position by several ligaments and peritoneal folds to the colon (splenocolic ligament), the stomach (gastrosplenic ligament), the diaphragm (phrenosplenic ligament), and the kidney, adrenal gland, and tail of the pancreas (splenorenal ligament) ( Fig. 1 ).
Wandering spleen occurs when the suspensory ligaments are congenitally absent or due to laxity of the suspensory ligaments. If a person is born with a wandering spleen that may be the result of a defect in a certain area of the developing embryo (mesogastrium dorsum) which gives rise to suspensory ligaments of the spleen. Acquired wandering spleen may occur during adulthood due to accident or injury, another underlying disorder (e.g., connective tissue disease), or the ligaments' abnormal relaxation (laxity) caused by pregnancy. The spleen could be located in the lower abdominal or pelvic cavity. As in our case spleen was located in the lower abdominal cavity and the pelvis ( Fig. 2 ).
Patient presentation could be asymptomatic, chronic left abdominal pain, or symptoms and signs of complication. The most common complication of wandering spleen is torsion [ 1 ]. Other complications are splenic infarction, splenic abscess, variceal hemorrhage, small bowel or gastric volvulus, and pancreatic tail necrosis [ 12 , [14] , [15] , [16] ]. Splenic torsion is when there is a twisting of the spleen along its vascular pedicle, subsequently leading to abdominal pain in the setting of organ ischemia. Vascular thrombosis and splenic infarction may follow splenic torsion. Evidenced by fatigue, weakness, lower GI bleeding, anemia, bloody vomit (hematemesis), and/or thrombocytopenia in our patient platelet level was 111,000 cells/μl which suggests vascular thrombosis [ 11 ].
The diagnosis and presentation of splenic torsion are variable and challenging during pregnancy. One of the challenges during pregnancy is diagnosis in that it may be misdiagnosed for other common gynecologic conditions like adnexal mass [ 17 ], ruptured ectopic pregnancy [ 18 ], or the symptoms of pregnancy [ 2 ]. Although most of the cases presents as an acute emergency, in some instances, the attack lasts from several days to months, the patients having survived the acute onset with adherence of omentum and intestine [ 2 ]. This case came with a complaint of sudden onset of colicky abdominal pain of three days' duration which is over the left lower quadrant of the abdomen. She had associated frequent episodes of non-bilious projectile vomiting of ingested matter. Abdominal examination showed a distended abdomen, with deep and rebound tenderness over the right lower quadrant and left lower quadrant of the abdomen. There was a palpable smooth-surfaced tender mass over the lower quadrants of the abdomen. CBC showed thrombocytopenia and leukocytosis with left shift while abdominopelvic ultrasound suggests a low-lying spleen located in the lower abdominopelvic cavity with no blood flow seen at the hilum. The spleen is homogeneously enlarged measuring 18.4 cm. Because of the typical description of abdominal ultrasound finding, we didn't consider having abdominal CT scan due to possible radiation exposure for the 1st trimester pregnancy [ 19 ]. With the above preoperative impression, the decision for surgery was made immediately. The other peculiarity during pregnancy is torsion of the spleen has higher mortality reaching up to 41 % [ 2 ] which may be from delay in diagnosis or misdiagnosis. There has been increased preoperative diagnosis of this condition in recent years and in the future data on mortality of splenic torsion during pregnancy may be demonstrated to be lower [ 4 ]. We recommend having a separate systemic review of the literature on splenic torsion during pregnancy.
One of the intraoperative challenges reported from the literature is the existence of adhesion between the small bowel and the spleen [ 2 ]. In our case, there was no adhesion gastric volvulus or pancreatic tail involvement.
Prevention of post splenectomy sepsis is achieved by three strategies which are Immunization, antibiotics and patient education [ 20 ]. Recommended immunoprophylaxis is for encapsulated bacteria like Pneumococcus, Hemophilus influenza B, and Meningococcus and viruses like influenzas virus [ 21 ]. In our case the vaccines found at time of request were polyvalent Pneumococcal vaccination and the conjugate Haemophiles influenza B vaccine. One of the difficulties we faced was getting vaccines. We used the free resources from the childhood immunization program after securing appropriate authority.
Oral antibiotics were prescribed up on discharge of the patient. Choice of oral antibiotic was oral penicillin which is the preferred prophylactic antibiotic for the prevention of post splenectomy sepsis [ 22 ]. Patient was given an education on prevention of post splenectomy sepsis and how to manage once it happens and on the need of life long follow-up.
4. Conclusion
Torsion of the spleen is an uncommon condition, which occurs more commonly in females than males. During pregnancy difficulties in diagnosis are likely to arise because the possibility of splenic torsion is not often considered as a differential, and it may be made more difficult by the presence of the physiologic symptoms of pregnancy. Unless clinicians depend on clinical symptom with high index of suspicion they easily are misdiagnosed for other Gynecologic emergencies like ovarian cyst, adnexal mass, or on account of symptoms relating to pregnancy which leads to delay in intervention that may lead to both maternal and fetal demise.
Written informed consent was obtained from the patient, in their native language, for publication of non-identifying information including accompanying intraoperative images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval is deemed unnecessary by the hospital ethical committee as this is a single case encountered during practice and it doesn't involve human or animal experiments.
No funding was provided for this case report.
Alemneh Mitku Chekol, MD.
Research registration number
Credit authorship contribution statement.
- Alemneh Mitku Chekol, MD -Primary operating surgeon, Study concept and design, writing the paper and literature review.
- Aemro Tadesse, MD -Editing of the paper and patient management, acquisition of data, and critical review of the paper.
- Seyoum Hailu Abebe, MD -Editing of the paper and patient management, acquisition of data, and critical review of the paper
- Zelalem Assefa Semagn, MD - Editing of the paper and patient management, acquisition of data and critical review of the paper.
- Barakad Mohammed Hassen, MD – involved in the patient management, acquisition of data and critical review of the paper.
Declaration of competing interest
No conflict of interest between the authors.
Torsion of wandering spleen
Affiliation.
- 1 Inonu University, Faculty of Medicine, Department of General Surgery, Malatya, Turkey. [email protected]
- PMID: 20120444
Wandering spleen is characterized by ectopic localization of spleen owing to the lack or weakening of the major splenic ligaments. In present study, two cases with torsion of wandering spleen were reported. The first case was a 30-year-old female who was admitted to emergency department with acute abdominal pain and vomiting. Abdominal Ultrasonography and computed tomography showed a round solid hypodense mass that was located in the left hypochondriac region of abdomen. At laparotomy, the patient was found to have torsion of a wandering spleen with complete infarction and pancreatic tail infarction. Splenectomy and distal pancreatectomy were performed. The second patient was a 19-year-old female. She was admitted to emergency department with abdominal pain. Axial computed tomography (CT) showed pelvic mass that indicated a possibility of a wandering spleen. The wandering spleen was removed with its long pedicle because of infarction. Torsion of wandering spleen must be considered in differential diagnosis of acute abdomen when a palpable painful abdominal mass is present on physical examination, and the spleen is absent in its normal anatomical location on radiological examination (Fig. 4, Ref. 8). Full Text (Free, PDF) www.bmj.sk.
Publication types
- Case Reports
- Torsion Abnormality / complications
- Torsion Abnormality / diagnosis*
- Wandering Spleen / complications
- Wandering Spleen / diagnosis*
- Young Adult

COMMENTS
Clinical presentation. A wandering spleen can be an elusive diagnosis as its presentation is greatly variable and intermittent torsion can cause non-specific signs and symptoms. It can present as an asymptomatic or painful abdominal mass, intermittent abdominal pain, or as an acute abdomen (e.g. bowel obstruction, acute pancreatitis) 3,4,6.
Wandering spleen is a rare condition that results from elongation or maldevelopment of the spleen's suspensory ligaments, which hold the spleen in its normal anatomical position in the left upper quadrant of the abdomen [ 3 ]. It can present with a torsion of its pedicle causing an acute abdomen, or it may be an incidental finding presenting ...
Symptoms of wandering spleen are typically those associated with an abnormally large size of the spleen (splenomegaly) or the unusual position of the spleen in the abdomen. Enlargement is most often the result of twisting (torsion) of the splenic arteries and veins or, in some cases, the formation of a blood clot (infarct) in the spleen.
Wandering spleen is a rare clinical entity seen mainly in male infants or women of reproductive age group (20-40 years), in which spleen is present at an ectopic location. [ 5, 6] This has been attributed to the laxity of splenic ligaments which can be congenital or an acquired weakness due to hormonal changes or multiple pregnancies. [ 7, 8, 9 ...
Wandering spleen (or pelvic spleen) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the ... removal of the spleen, are performed due to having this disorder. In 1992, the youngest case of the literature of torsion of wandering spleen at two days of birth was reported in Lebanon, by Dr Edouard Sayad ...
Abstract. Wandering spleen is a rare condition defined as a mobile spleen only attached with its pedicle. It can be complicated by a volvulus, which is a surgical abdominal emergency. Preventing infarction is the aim of a prompt surgery that can preserve the spleen and then proceed to splenopexy. We report a rare case of torsion of a wandering ...
Wandering spleen (or ectopic spleen) is a rare anomaly resulting from hyperlaxity or even absence of the ligaments that hold the spleen in its anatomical position. Although more frequently a congenital condition, it can also be acquired. Torsion of the vascular pedicle is its potential main complication with subsequent development of splenic infarct. In this paper we will describe the ...
Wandering spleen is a rare condition in which the spleen migrates from its usual anatomical position, commonly to the lower abdomen or pelvis. Wandering spleen is rare, with a reported incidence of <0.5%. It can present as an asymptomatic or painful abdominal mass, intermittent abdominal pain, or as an acute abdomen due to torsion 1,2.
Wandering spleen (or ectopic spleen) is a rare anomaly resulting from hyperlaxity or even absence of the ligaments that hold the spleen in its anatomical position. Although more frequently a congenital condition, it can also be acquired. Torsion of the vascular pedicle is its potential main complica …
Total or partial absence of parenchymal enhancement is indicative of poor perfusion (Figs. 4, 5, 6 and 7) and is an indirect sign of pedicle torsion and secondary infarct. The whirl sign is con-sidered a highly specific radiological finding of torsion of the pedicle of a wandering spleen.
Wandering spleen can be found on imaging studies as a spleen that is located somewhere other than it's usual position in the left upper abdomen. This article will discuss diagnosis, complications and treatment of wandering spleen. ... In cases where the spleen becomes twisted (torsion), symptoms can quickly escalate to sharp abdominal pain ...
A wandering spleen (WS) is a rare clinical entity characterized by a spleen located in the lower part of the abdomen or the pelvic cavity rather than the normal anatomical site. The complications of a wandering spleen include splenic torsion, splenic infarction, and adjacent visceral injury.
The presence of wandering spleen with torsion of the vascular pedicle was confirmed at laparotomy in both instances. Splenectomy was performed in both cases with good recovery. Conclusion: Torsion of a wandering spleen poses a diagnostic challenge. A high level of suspicion is required to make a diagnosis and institute appropriate treatment.
Torsion of a wandering spleen is a rare but fulminant condition and is part of the differential diagnosis in patients presenting with acute abdominal pain. It results due to absence or laxity of the various ligaments supporting the spleen. Patients may be asymptomatic or may present with acute abdominal pain.
The torsion of wandering spleen is a rare clinical condition. Case report: We evaluate a case diagnosed with torsion of wandering spleen and underwent splenectomy in our hospital and discuss it in light of the literature. A 26-year-old man presented to the emergency department with abdominal pain and abdominal distention.
Wandering spleen is a rare entity in which the spleen is hypermobile and ectopic in position, and attached only by an elongated vascular pedicle which becomes prone to torsion. Wandering spleen is found in less than 0.5% of splenectomies and occurs mainly in children and women aged 20-40 years [ 4 ]. This condition is a result of congenital ...
Wandering spleen is a very rare defect characterized by the absence or weakness of one or more of the ligaments that hold the spleen in its normal position in the upper left abdomen. Patient symptomatology is variable and ranges from mere feeling of an abdominal lump to sudden abdominal pain due to infarction. Patients may have subacute to chronic abdominal or gastrointestinal complaints ...
Anatomical variation of the spleen's position in the abdomen, is a rare condition called Wandering Spleen (WS). WS is a vital differential diagnosis in patients presenting with acute abdomen. Concerning the high incidence of splenic torsion in these patients, early recognition is important. We report two cases of this rare condition ...
Torsion of the wandering spleen is a rare condition usually unsuspected preoperatively. In previously reported cases in the past, attempts at splenopexy have failed and splenectomy has been regarded as the treatment of choice. We are presenting two children with splenic torsion. In one complete infarction of the spleen had occurred and so ...
Wandering spleen is when the spleen is in an ectopic position due to laxity of the anchoring ligaments. This results in a long splenic pedicle, predisposing the patient to splenic torsion, leading to partial or complete infarction .. The presentation of wandering spleen varies widely from abdominal mass, ranging from intermittent abdominal pain to being asymptomatic, found by incidental ...
Abstract. Wandering spleen is a rare condition that accounts for less than 0.25% of all indications for splenectomy. It is characterized by ectopic localization of the spleen owing to the lack or weakening of its ligaments. Torsion is the most common complication due to its long pedicle and high mobility, which may result in acute abdomen.
The most common complication of wandering spleen is torsion and other complications are splenic infarction, splenic abscess, variceal hemorrhage, gastric volvulus, and pancreatic tail necrosis [4, 5, 7]. There are few reports of wandering spleen torsion in pregnant mothers . The diagnosis and presentation of splenic torsion are variable and ...
Wandering spleen is characterized by ectopic localization of spleen owing to the lack or weakening of the major splenic ligaments. In present study, two cases with torsion of wandering spleen were reported. The first case was a 30-year-old female who was admitted to emergency department with acute abdominal pain and vomiting.