WWW.PRIMECLINICAL.COM
UB ENCOUNTER CONDITION CODES
These codes are required for completion of the form CMS-1450 for billing.
Form Locators (FLs) 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, and 28 are Condition Codes.
Situational . The provider enters the corresponding code (in numerical order) to describe any of the following conditions or events that apply to this billing period.
Codes used for Medicare claims are available from Medicare contractors. Codes are also available from the NUBC ( www.nubc.org ) via the NUBC's Official UB-04 Data Specifications Manual.
Code Title Definition
Top of Page


Adjustment condition code clarification
It is very important to use the most appropriate condition code when adjusting claims.
Condition codes
Condition code D1
Condition code D9
Condition code quick reference
2021 E/M Guidelines: Understanding Total Visit Time
In this episode of the Listen-Up Series on 2021 E/M Guidelines , Lori Cox is joined by Elizabeth Hylton to talk about total visit time. They'll share how to correctly document the time you spend in patient care, what you can count and can't count on in E/M selection, and how to stand up to payer and auditor scrutiny. Plus, they discuss real-life office visit scenarios and answer questions like:
How is the new total visit time defined and what activities can be counted toward that total time?
What is the difference with the CMS prolonged services?
Can you explain the new HCPCS code G2211?
Are there guidelines on which calculation to use, MDM or time?
When time is documented, does time trump MDM?
Plus, they discuss AMA guidelines, the difference between the time standards and calculations, and more. This webinar will provide a better understanding of what to expect in provider notes and how to ensure compliant documentation.
To read the full conversation, check out the transcript below.
Who would benefit from watching this webinar?
Medical Billers
Medical Billing Managers (including Supervisors, Directors of Billing, etc.)
Medical Coders
Medical Coding Educators / Trainers
Medical Coding Managers (including Supervisors, Directors of Coding, etc.)
Medical Auditors
Healthcare Documentation Specialists
Documentation and Coding Managers / Directors
Healthcare Office Managers
Presented by

Stephani Scott
Cpc, rhit / vice president of audit services / aapc /.
Stephani Scott has over 30 years of experience in the healthcare industry working closely with physicians and staff in Health Information Management. She has worked in a variety of settings including hospitals, long-term care, large multispecialty physician practice, and EHR software design and development. Scott was a part owner of a consulting company for many years providing services in best practices for physician practice management services including coding and documentation audits, compliance, and revenue cycle management. She has extensive experience in inpatient and outpatient auditing and coding compliance. Throughout her career, Scott has enjoyed teaching E/M coding, compliance, and EMR utilization to many physicians and staff locally and nationally.

Elizabeth Hylton
Cpc, cemc / aapc services regional director.
Elizabeth Hylton began her coding career by identifying claims submission errors involving ICD-9 and CPT® codes on hospital claims. From there, she worked as a Charge Entry Specialist for a local family medicine practice. She worked her way up to Coding Tech I at Carolinas Medical Center- Northeast submitting claims for half of the team of 22 hospitalists and 8 Critical Care providers. From there, she accepted a position at Sanger Heart and Vascular Institute as a Front Desk Clerk who also functioned as the backup Coding Tech. She obtained her CPC in December of 2011 and in March of 2012 accepted a position as an Auditor/Educator for Carolinas HealthCare System. She went on to support 126 physicians in 22 practices with specialties that included Dermatology, Endocrinology, Gastroenterology, Hematology/Oncology, Internal Medicine, Orthopedic Surgery, Pediatrics, Cardiology, and Concierge Medicine. She obtained her CEMC certification in May of 2014. In January of 2015 she was offered a position as Business Office Supervisor for one of the larger physician groups within Carolinas HealthCare System, where she gained experience with Lean, and remained until she accepted the position of Director of Client Engagement with the AAPC Services in July of 2015 through September 2021.
Full Transcript
Stephani : Welcome, everybody, to our Listen-Up Series on 2021 E/M Guidelines. Today, we're going to be talking about total visit time. My name is Stephani Scott, and I will be your host today. I have worked in the healthcare industry for over 25 years. During that time, I've had the pleasure of working in a variety of different settings, including acute hospital, long-term care, large multi-specialty physician groups, and I've worked for a major EMR vendor doing design and development work. For several years, I was a part-owner of a consulting company in which we provided services for physician practice management, including coding, billing, and revenue cycle. Currently, I am the vice-president for AAPC's audit services. My guest today is Elizabeth Hylton. Elizabeth, will you introduce yourself?
Elizabeth : Absolutely. I am a regional director with AAPC Audit Services Group. I have about 17 years’ experience in the healthcare administration setting. I hold the credentials of CPC and CEMC, and I've had the privilege of working pretty much every line of service in the admin field of healthcare. I started off as a front desk person in a family practice clinic, and gradually worked my way through the revenue cycle, from denials all the way to claims processing, and then auditing in a retrospective manner. So, I've pretty much done it all. If you can do it administratively in healthcare, I've done it.
Stephani : Well, that's great. You're perfect one to join me today for our webinar. Okay. First, what we thought we would do is talk about the new time-based definition and how the calculations work. Then I actually pulled some real-life office visit scenarios. Obviously, we've redacted them and tweaked them just a little bit, but these are scenarios that we've come across over the last several months. And then finally, Elizabeth, I wanted to go over some common questions that we keep getting from different organizations.
Elizabeth : Sounds great.
Stephani : So, okay, perfect. With that, let's go ahead and get started. So we now have these two different time standards and calculations. Elizabeth, can you tell us what are the difference between these two?
Elizabeth : Absolutely. So, under the system we're used to, '95/'97 guidelines, we had to put a statement in there that showed we spent greater than 50% of a total visit face-to-face with our patient counseling and coordinating care. Now, this is still going to be the case with our other E/M categories, just not the office and outpatient setting. For that under our new 2021 calculation, it is going to be based just on total visit time on the day of the patient encounter. So much, much simpler in the office and outpatient world.
Stephani : Okay. Thank you. So Elizabeth, tell us exactly how this new total visit time is defined and what activities can be counted towards that total time.
Elizabeth : That's a great question. So total time is being defined as what is spent on the day of the patient encounter. It is going to include both face-to-face and non-face-to-face activities. And we have it broken down on the slide here that we're referencing. We have things that we can include and things we can't include. So things we can include, prep on the same day, obtaining and reviewing history from our patient's records, the exam that we perform with them, any counseling and ordering of tests, medications, and procedures, okay? So things that are typically associated with the evaluation and management service that our providers historically have not been able to count like their prep work.
Charting is also included on this, care coordination. All of those services that previously we couldn't really get credit for because they didn't take place face-to-face with the patient, now we can include. And no longer do we need to use the statement of greater than 50% of time was spent in counseling. It's just the total time that you spend taking care of your patient on that day.
Stephani : Okay. So what types of activities are not included?
Elizabeth : So some of the things that we would not include, we have to bear in mind that this is provider time only. It is not going to count staff time. It is not going to count the separately reported tests or procedures that you perform on the day. So if there's a CPT code associated with something that you're doing outside of the evaluation and management service, the time that you spend performing those identified CPT codes is not included. Slow charting is also not something that you would include.
I had a practice who was getting ready to go to a new EMR system in February. And they're very concerned about having two learning curves to come up to, but we had to make sure we were very clear there's a reasonable expectation surrounding how long it takes to chart, and that's what we count. Not necessarily coming up to a learning curve in an EMR. And then, of course, any elements that are performed on a different date. So depending on your provider's flow and the way they like to practice medicine, if they are doing prep work the day before they see a patient or they're doing review the day after they see a patient, those elements will not count. It has to be elements that are performed on the same calendar date as the patient encounter.
Stephani : Okay. Great. That's some good insight. Okay. On this slide deck, we've broken out the different time ranges. So Elizabeth, kind of walk us through the ranges for new patient and established patient.
Elizabeth : Okay. This is the first time when I reviewing these guidelines initially that I went, "Whoa, that's different," because we're very used to seeing a static point in time assigned to these codes. You know, it's been very easy for me previously to just rattle off, "Oh yeah, you need 15 minutes for a 99213," or, "You need 25 minutes for a 99214." That's not the case anymore. Now it's defined by a range of time and your static point will fall into this range.
So as you can see, there's kind of a pattern with this. New patients are gonna start at 15 minutes and they're gonna go up in 15-minute increments. So once you hit 30 minutes, you're at a 99203, once you hit 45, you're at a 99204, 60 for 99205, and so on versus under the established patient rules, we have to start with 10 minutes for a 99212, and then we billed in 10-minute increments. You start with a 99213 once you hit 20 minutes, 30 minutes for a 99214, and so on.
So we've been encouraging our providers, you know, you have to understand you're now being defined by a range of time, but please do not document a range of times. Tell us the static amount of time that you spent with your patient on this day, and then a coder will assign the appropriate E/M based on what you're telling us in documentation.
Stephani : Okay. Great. So there has been some confusion on whether or not CMS has adopted these time ranges. Can you help us with that?
Elizabeth : From my understanding, they have adopted this. This is in the CPT books for 2021. The only place where CMS kind of gets a little different from AMA is going to be with calculation of prolonged services. Those rules are a little bit different.
Stephani : Okay. Thanks for clarifying. Let's go ahead and talk about the prolonged services. So Elizabeth, help us define the AMA's guideline here.
Elizabeth : All right. So AMA has released a new code for 2021 CPT code set, and this is 99417. This will define 15 minutes of prolonged office or other outpatient evaluation and management services beyond the total time of the primary procedure which has been selected using total time. So we can only use these with 99205 and 99215 only, okay? These are not going to apply to the remainder of the office and outpatient code set. We have to remember that for our other categories, we're still going to continue to use the prolonged services codes we're used to seeing represented by the range of 99354 to 99359, 99415 and 99416.
So, CPT has given us some really good examples of how to calculate this when we're reporting 99417, an initial time unit of 15 minutes should be added once the minimum time in the primary E/M code has been surpassed by that 15 minutes. So, for example, we're not gonna report 99417 until at least 15 minutes of time beyond 60 minutes i.e., 75 minutes has been accumulated. The same is true for 99215. We have to get to 15 minutes past 40 minutes or 55 minutes before we can bill prolonged services.
Stephani : Okay. So on this slide, we've got those time ranges for prolonged new patient and prolonged established patient. Now, does the times stop, the prolonged time maximum stop at the four units that I have listed on the slide, or does that continue on?
Elizabeth : It can continue based on how much time is being spent with the patient, and it does not have to be contiguous, it can be incremental. So let's say you spend 40 minutes this first hour, and then you come back to the patient later in the day and you're spending more time. All of it is cumulative. Again, based on the date of service of the patient encounter. So if you're spending units past four, then we just have to remember it's in 15-minute blocks. So we have to balance how much time is being spent in what we're describing in our notes versus math here. So we have to make sure that those two things are lining up, but you can bill past four units.
Stephani : Okay. All right. Thank you. So now tell us what the difference is with the CMS prolonged services.
Elizabeth : All right. So Medicare has decided to assign a status indicator of invalid to CPT 99417. Meaning if you were to bill that code to CMS, they would not return payment for it. Instead, they have adopted their own HCPCS code for this, which is G2212. The description is similar. It's the prolonged office or other outpatient evaluation and management services beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service, each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient context.
And the thing we have to remember here is this code kicks in for time beyond the maximum required time of the primary procedure. Once again, it can only be used with 99205 and 99215. You will not be able to report this code on the same date of service as our other prolonged services codes, 99354 to 99359, 999415, and 99416. And we have to remember we cannot report G2212 for any time unit less than 15 minutes. There is not a midpoint to this code. We have to satisfy 15 full minutes before we can bill it.
Stephani : Okay. So on this slide, we've broken out those specific time ranges. So, for example, if I'm looking at a new patient record and my total time were 90 minutes for CMS, could I also bill 99205 and the G2212 with one unit?
Elizabeth : So based on this, if we have a new patient for 99205, we would not be able to bill the G2212 because we've not surpassed that 15-minute mark. Well, wait a minute, hold on. Let me look at this. It's early in the morning, my brain is not massing correctly. So G2212 does describe that range of time. If we look at 99205, it does appear based on this table, we will be able to bill the G2212 on 90 minutes for a new patient. What we have to remember is that the full 15 minutes are past the max time of the code.
So, whereas we are looking at less time under the AMA guidelines, Medicare requires more. My rule of thumb talking to these providers is that you have to hit at least 15 minutes past the maximum amount of time for this code before you even consider upending G2212. And that's true for both new and established categories.
Stephani : Okay. So the 89 minutes is that 15-minute mark for new, and the 69 is that 15-minute mark for 50. Okay. Got it.
Elizabeth : Correct.
Stephani : Thank you. All right. So CMS released this new HCPCS code G2211, and we have just been getting a ton of questions about this new code and how practices can get paid for it. So, Elizabeth, can you help us better understand this new code?
Elizabeth : Sure, absolutely. This is something that CMS released to describe visit complexity that was inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed healthcare services and/or with medical care services that are part of ongoing care related to a patient's single, serious condition or a complex condition. The spirit of the code was great. And when I read this, I instantly thought, wow, this is like the spirit of transitional care management without actually having to have the inpatient admission associated with it and all the rules that go with that code set. This is wonderful. It's gonna describe additional time, intensity, and practice expense for services that are building that longstanding relationship and addressing the majority of patient healthcare needs over time.
This is exactly what we're seeing with some of our older population. They have multiple chronic conditions that are being evaluated and the physician should be compensated for the care relating to those conditions. But then literally at the 11th hour, 2:00 a.m. on December 1st, Medicare came back and said, "We're not going to price this code. It is not going to be effective for payment until January 1st, 2024." So we have to wait on this for about three more years, and then we will be able to account for increased visit complexity.
Stephani : Okay. Thank you. A little disappointing we're not able to use it yet, but it's good that it's coming in the future. Something to look forward to, for sure.
Elizabeth : Absolutely.
Stephani : Okay. So let's go over some scenario. So Elizabeth, I'm just gonna pass this directly over to you.
Elizabeth : Okay. Fantastic. So let's talk about a patient. Their chief complaint is going to be a goopy eye. Their mom reports the patient woke up with left eye matted shut. The eye is itchy and watery. The mother denied the patient having any fever, ear pain, rhinorrhea, or rash. Patient's not on any medication. The provider documents an exam of vision, right 10 out of 10, left 10 out of 13, eye is injected, pupils equal round reactive to light and accommodation, extraocular movement's intact, no periorbital edema, or erythema, or tenderness. And then they give an assessment of conjunctivitis. They give a prescription for Polytrim drops, three drops to the affected eye five times a day for seven days. And we instructed the mom to call if the patient develops a fever. Provider also denotes a total visit time of 12 minutes. So based on that documentation of time, we are going to have a 99212 as our level.
Stephani : Okay. Perfect. Now I noticed on that time, all it says is just the minutes, the total visit time 12 minutes. Is that gonna suffice the documentation requirement? Don't we have to put more to that?
Elizabeth: It's minimally acceptable. Now me as an auditor, my brain does a thing where I would probably want to see more, but the provider is saying that the total visit time on the date of service is 12 minutes. So it is sufficient. If it were me, I would probably educate them to flesh that out just a little bit. Total visit time spent in E/M service exclusively 12 minutes, and you're good to go.
Stephani : Okay. So this next scenario kind of addresses that. Can you help us walk through it?
Elizabeth : Absolutely. So we have a statement that the provider spent greater than 45 minutes with the patient and greater than 50% of that counseling on diagnosis treatments, previous test results, histories, and updating EMR as described above. Now that is absolutely textbook from a 1995/1997 documentation standpoint. For 2021, we're gonna switch that up a little bit. And the provider will now document, "A total of 60 minutes was spent today reviewing the patient's diagnostic tests, assessing and examining the patient and documenting. None of this time was spent performing separately billable procedures or ancillary services.
So what the provider does well with this 2021 is he gives us the exact total time that was spent with the patient. He avoided language like at a minimum or approximately. It was 60 minutes that was spent today. So he's letting us know this was all spent on the day of the patient encounter. The documentation of what was performed ideally is going to be patient-specific. Now I underlined this on my notes, reviewing patient's diagnostic tests, assessing and examining the patient and documenting, that is not a requirement of 2021.
However, many organizations that I've provided this training to, they have adopted it from a best practice standpoint to support individuality from one patient to the next. I would caution our providers to be careful of using templates that look identical from one patient to the next. Copy-paste is still going to be a concern in 2021. And I suspect given time is one of only two components used for selecting levels in the office and outpatient setting, time-based billing is going to come under even greater scrutiny. So we have to be careful that what we're saying we're doing from a time perspective is backed up with what's actually being done in documentation.
Stephani : That's some good advice, Elizabeth. Thank you. Okay. So we have a third scenario with a prolonged time. Can you walk us through this one?
Elizabeth : Sure. So we have an established patient here, so we're already going to be looking at our...if we're planning on doing a prolonged service, it's gotta be at least a 99215. The patient presents with fluid retention and shortness of breath. The assessment and plan diagnose this patient with congestive heart failure. The provider goes on to say that they spent 62 minutes obtaining records from primary care, evaluating their patient, and discussing treatment options to include fluid restriction, a low-salt diet, and compression hose.
If the patient continues to retain fluid, we'll consider low-dose Lasix. So under the AMA guidelines, this is enough to substantiate both the 99215 and one unit of 99417. Given the fact this was congestive heart failure, I instantly think this is probably a Medicare-aged patient, and under CMS rule, this will only substantiate a 99215. It will not meet the threshold in order to bill the additional 99417, or in the Medicare patient's case, the G2212.
Stephani : All right. Thank you, Elizabeth. Yep. So let's move on to some common questions that we keep getting. So I'll go ahead and read the questions. Are there guidelines on which calculation to use, MDM or time?
Elizabeth : The guidelines that we have specifies that an E/M service should be selected based on either MDM or time? So whichever one is beneficial to the provider, if the provider substantiate their level on time, MDM does not also have to be documented and vice versa. If the time and MDM are both documented and they can split, so let's say one component supports a lower level than the other, we'll use whichever component is beneficial to the provider.
Stephani : Okay. So the next question is when time is documented, does time trump MDM?
Elizabeth : This is a great question. Not always is the answer. For example, if by time a provider supports a 99213, let's say they spent 20 minutes with their patient, but the medical decision-making supports a level four because they have management of two stable chronic conditions with moderate risk to the patient, and the provider bills that level four, the level is supported by their medical decision-making as outlined in documentation. There was initially some discussion amongst providers that they just bill based on time since it was easier. And if that's all they have to put in their note, cool, that's what we're gonna do.
And we had to remind our providers you have to understand, in some cases, they'd be selling themselves short because of how time had been restructured now with that range instead of a static point, but to bill based solely on time would actually hurt their bottom line. So time does not always trump MDM. And I don't feel like if a provider substantiates a greater level of MDM, it would be fair to rely on the time. Their cognitive work is right there on the paper for us to see, and it may exceed the amount of time that was spent.
Stephani : Thank you. That's some great insight. So our last question is if MDM supports a 99215, however, the total visit time supports a 99214, should 99214 be reported to avoid reporting a level five as a target? So we all know about the E/M bell curve and the watchful eyes of the payers on those higher levels. So in this case, what should we do?
Elizabeth : Well, I tend to take those bell curves with a grain of salt. They are excellent tools to establish a baseline and a benchmark and help our providers understand what their colleagues nationwide are doing. However, at some point, we have to stop thinking about those higher levels as a target that we don't want on our backs. If a provider is supporting their MDM complexity, we have to allow credit for the cognitive work that's associated with the complexity and risk. Usually, when I'm auditing, I'm looking at the medical decision-making first because that's really the clinical determination that the provider is making. And then I'll use time as a fallback if I need it.
I will very rarely look at time and pull a provider's level down, especially if he's given me a beautiful description of a high MDM. To me, that's an unfair penalty and way too stringent of a stance. So if they support their MDM but their time supports a lower level, I would go with MDM because once again, that's measurement of the provider's cognitive effort on paper and they should be giving credit for the work that they're performing.
Stephani : That's excellent advice. Well, this concludes our Listen-Up Series on the 2021 E/M Guidelines, understanding total times for those guidelines. Elizabeth, thank you so very much for being my guest. And thank you, everyone, for joining us. Have a great day.
Want more than this webinar?
Our experts are standing by, ready to help you with challenges related to E/M guidelines, claim denials, data files, staff training, and more.
You might also like
- Evaluation and Management
- Documentation
- Business Solutions
Have a question?
Better revenue starts here..

Medicare codes
Nov 16, 2009 | Medical billing basics | 1 comment
D1 Claim/service denied. Level of subluxation is missing or inadequate. D2 Claim lacks the name, strength, and dosage of the drug furnished. D3 Claim/service denied because information to indicate if the patient owns the equipment that requires the part or supply was missing. D4 Claim/service does not indicate the period of time for which this will be needed. D5 Claim/service denied. Claim lacks individual lab codes included in the test. D6 Claim/service denied. Claim did not include patient’s medical record for the service. D7 Claim/service denied. Claim lacks date of patient’s most recent physician visit. D8 Claim/service denied. Claim lacks indicator that “xray is available for review.” D9 Claim/service denied. Claim lacks invoice or statement certifying the actual cost of the lens, less discounts or the type of intraocular lens used. D10 Claim/service denied. Completed physician financial relationship form not on file. D11 Claim lacks completed pacemaker registration form. D12 Claim/service denied. Claim does not identify who performed the purchased diagnostic test or the amount you were charged for the test. D13 Claim/service denied. Performed by a facility/supplier in which the ordering/referring physician has a financial interest.
Remark codes must be used to relay service-specific Medicare informational messages that cannot expressed with a reason code. Medicare remark codes are maintained by HCFA. Remark codes and messages must be used whenever they apply. Although contractors may use their discretion to determine when certain remark codes apply, they do not have discretion as to whether to use an applicable remark code in a remittance notice. A limitation of liability message (m25-M27) must be used where applicable. An unlimited number of Medicare line level remark codes may be entered as warranted in an X12 835 Remittance Advice; there is a limit of 5 line level remark code entries in a NSF Remittance Advice and on a standard paper remittance notice. a. Line Level Remark Codes Code Value Description
M1 X-ray not taken within the past 12 months or near enough to the start of treatment. M2 Not paid separately when the patient is an inpatient. M3 Equipment is the same or similar to equipment already being used. M4 This is the last monthly installment payment for this durable medical equipment. M5 Monthly rental payments can continue until the earlier of the 15th month from the first rental month, or the month when the equipment is no longer needed. M6 You must furnish and service this item for as long as the patient continues to need it. We can pay for maintenance and/or servicing for every 6 month period after the end of the 15th paid rental month or the end of the warranty period. M7 No rental payments after the item is purchased, or after the total of issued rental payments equals the purchase price. M8 We do not accept blood gas tests results when the test was conducted by a medical supplier or taken while the patient is on oxygen. M9 This is the tenth rental month. You must offer the patient the choice of changing the rental to a purchase agreement. M10 Equipment purchases are limited to the first or the tenth month of medical necessity.
Medicare denial reason code -1 Medicare denial reason code – 2 Medicare denial reason code – 3 Denial EOB Medicare EOB Denial claim example Denial claim Medicare denial codes For full list
M1 X-ray not taken within the past 12 months or near enough to the start of treatment.
Why am I getting this rejection? How do I get paid?
Medical Billing Update
- Insurance denial code full List – Medicare and Medicaid
- Late filing reduction and Time Limits for Filing Part B Medicare Claims
- Ask people to take pictures for you
- Can PCP disenroll a patient from the memebr panel list
- Can we billed Medicaid patient for Medicare coins ?
Recent Posts
- Origin and Destination modifiers in Ambulance billing
- CPT code 88120, 81161 – 81408 – molecular cpt codes
- Denial – Covered by capitation , Modifier inconsistent – Action
- CPT code 10040, 10060, 10061 – Incision And Drainage Of Abscess
- CPT Code 0007U, 0008U, 0009U – Drug Test(S), Presumptive
- Medical billing basics
All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. All the information are educational purpose only and we are not guarantee of accuracy of information. Before implement anything please do your own research. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail dot com. We will response ASAP.

Jurisdiction E - Medicare Part A
California, Hawaii, Nevada, American Samoa, Guam, Northern Mariana Islands
- Noridian Medicare Portal (NMP) Login
OPPS Payment Status Indicators - JE Part A

Browse by Provider Type
- Acute Inpatient Prospective Payment System (IPPS) Hospital
- Critical Access Hospital (CAH)
- Comprehensive Outpatient Rehabilitation Facility (CORF)
- End Stage Renal Disease (ESRD)
- Federally Qualified Health Center (FQHC)
- Fee-for-Time Compensation Arrangements and Reciprocal Billing
- Inpatient Psychiatric Facility (IPF)
- Inpatient Rehabilitation Facility (IRF)
- Long Term Care Hospital (LTCH)
- Mental Health
- Military Treatment Facility (MTF)
- Nonphysician Practitioner (NPP)
- Outpatient Prospective Payment System (OPPS)
- Outpatient Therapy
- Provider Based Facilities
- Rural Emergency Hospital (REH)
- Rural Health Clinic (RHC)
- Skilled Nursing Facility (SNF)
- Sleep Medicine
OPPS Payment Status Indicators
- CMS Addendum A and Addendum B Updates
© 2024 Noridian Healthcare Solutions, LLC Terms & Privacy
End User Agreements for Providers
Some of the Provider information contained on the Noridian Medicare web site is copyrighted by the American Medical Association, the American Dental Association, and/or the American Hospital Association. This includes items such as CPT codes, CDT codes, ICD-10 and other UB-04 codes.
Before you can enter the Noridian Medicare site, please read and accept an agreement to abide by the copyright rules regarding the information you find within this site. If you choose not to accept the agreement, you will return to the Noridian Medicare home page.
THE LICENSES GRANTED HEREIN ARE EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THESE AGREEMENTS. BY CLICKING ABOVE ON THE LINK LABELED "I Accept", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THESE AGREEMENTS.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK ABOVE ON THE LINK LABELED "I Do Not Accept" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THESE AGREEMENTS CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
LICENSE FOR USE OF "PHYSICIANS' CURRENT PROCEDURAL TERMINOLOGY", (CPT) FOURTH EDITION
End User/Point and Click Agreement:
CPT codes, descriptions and other data only are copyright 2002-2020 American Medical Association (AMA). All Rights Reserved. CPT is a trademark of the AMA.
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials: Local Coverage Determinations (LCDs), training material, publications, and Medicare guidelines, internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the AMA holds all copyright, trademark, and other rights in CPT.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized here in must be obtained through the AMA, CPT Intellectual Property Services, 515 N. State Street, Chicago, IL 60610. Applications are available at the AMA Web site, https://www.ama-assn.org .
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2)(June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a)(June 1995) and DFARS 227.7202-3(a)June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department Federal procurements.
AMA Disclaimer of Warranties and Liabilities CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. The AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. The AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with Noridian Healthcare Solutions or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product.
CMS Disclaimer The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of the CMS. The CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. The CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
This license will terminate upon notice to you if you violate the terms of this license. The AMA is a third-party beneficiary to this license.
LICENSE FOR USE OF "CURRENT DENTAL TERMINOLOGY", ("CDT")
End User/Point and Click Agreement
These materials contain Current Dental Terminology, (CDT), copyright © 2020 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
1. Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use CDT only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
2. Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CDT for resale and/or license, transferring copies of CDT to any party not bound by this agreement, creating any modified or derivative work of CDT, or making any commercial use of CDT. License to use CDT for any use not authorized herein must be obtained through the American Dental Association, 211 East Chicago Avenue, Chicago, IL 60611. Applications are available at the American Dental Association web site, http://www.ADA.org .
3. Applicable Federal Acquisition Regulation Clauses (FARS)\Department of Defense Federal Acquisition Regulation Supplement (DFARS) Restrictions Apply to Government use. Please click here to see all U.S. Government Rights Provisions .
4. ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
5. CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT should be addressed to the ADA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
LICENSE FOR NATIONAL UNIFORM BILLING COMMITTEE ("NUBC")
Point and Click American Hospital Association Copyright Notice
Copyright © 2021, the American Hospital Association, Chicago, Illinois. Reproduced with permission. No portion of the AHA copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA copyrighted materials including the UB-04 codes and descriptions may not be removed, copied, or utilized within any software, product, service, solution or derivative work without the written consent of the AHA. If an entity wishes to utilize any AHA materials, please contact the AHA at 312-893-6816
Making copies or utilizing the content of the UB-04 Manual or UB-04 Data File, including the codes and/or descriptions, for internal purposes, resale and/or to be used in any product or publication; creating any modified or derivative work of the UB-04 Manual and/or codes and descriptions; and/or making any commercial use of UB-04 Manual / Data File or any portion thereof, including the codes and/or descriptions, is only authorized with an express license from the American Hospital Association.
To obtain comprehensive knowledge about the UB-04 codes, the Official UB-04 Data Specification Manual is available for purchase on the American Hospital Association Online Store . To license the electronic data file of UB-04 Data Specifications, contact AHA at (312) 893-6816. You may also contact AHA at [email protected] .
Consent to Monitoring
Warning: you are accessing an information system that may be a U.S. Government information system. If this is a U.S. Government information system, CMS maintains ownership and responsibility for its computer systems. Users must adhere to CMS Information Security Policies, Standards, and Procedures. For U.S. Government and other information systems, information accessed through the computer system is confidential and for authorized users only. By continuing beyond this notice, users consent to being monitored, recorded, and audited by company personnel. Unauthorized or illegal use of the computer system is prohibited and subject to criminal and civil penalties. The use of the information system establishes user's consent to any and all monitoring and recording of their activities.
Note: The information obtained from this Noridian website application is as current as possible. There are times in which the various content contributor primary resources are not synchronized or updated on the same time interval.
This warning banner provides privacy and security notices consistent with applicable federal laws, directives, and other federal guidance for accessing this Government system, which includes all devices/storage media attached to this system. This system is provided for Government authorized use only. Unauthorized or improper use of this system is prohibited and may result in disciplinary action and/or civil and criminal penalties. At any time, and for any lawful Government purpose, the government may monitor, record, and audit your system usage and/or intercept, search and seize any communication or data transiting or stored on this system. Therefore, you have no reasonable expectation of privacy. Any communication or data transiting or stored on this system may be disclosed or used for any lawful Government purpose.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Read Your Healthcare Provider's Prescription
Parts of a prescription, prescription example.
- Newer and Simpler Information
What to Do if You Can’t Read It
A modern doctor's prescription is often digital, and you may not see it when sent from your healthcare provider directly to the pharmacy. For some controlled substances, digital prescriptions are even required. But when you need to read a prescription, it can still be pretty hard to decipher.
Knowing how to read a prescription will help you understand the meanings of various notations about what drug to use, how it should be dispensed, and how and when to take your medication.
This article will help you understand the abbreviations included when your healthcare provider writes a prescription. You'll be better equipped to decode a prescription or ask questions , which can help you avoid a medication error and give you better insight into your treatment.
Rockaa / Getty Images
A prescription is always written in a specific way. It identifies you and your healthcare provider, lists the specific medication prescribed, and includes details such as how to take the medication.
Identification
A prescription will always identify the healthcare provider who ordered the medication and the person who needs it. Your first and last name, along with a date of birth, are displayed. Some states require an address.
Some of the provider's information will be obvious to you, such as the name and office you visit. Other elements, including the license number, may be unfamiliar. You may see a National Provider Identifier (NPI) number, which is issued by the Centers for Medicare & Medicaid Services.
If your prescription is for certain controlled substances, it also will include a Drug Enforcement Administration (DEA) registration number.
Medication: The Rx Details
Your prescription (marked by the Rx symbol) needs to include the type of medication, typically with both the brand name and a generic name, when available. For example, a prescription for the common cholesterol medication Lipitor ( atorvastatin ) may carry both names, but the instructions for filling with a generic are included.
This part of the prescription also includes the strength of the drug (how many milligrams, for example) and the tablet, capsule, or other form in which your healthcare provider wants you to take it. A note called "Disp" refers to this information about how the drug should be dispensed.
The information includes how often you take your medication and the reason for it, called the indication. This is often on the same line as "sig," an abbreviation for the Latin word signetur that refers to the written instructions.
These are some of the notations about how to take medication that are commonly found on prescriptions:
- PO means orally
- QD means once a day
- BID means twice a day
- QHS means before bed
- Q4H means every 4 hours
- QOD means every other day
- PRN means as needed
- a.c. means before a meal
- p.c. means after a meal
Abbreviations about the route of administration (how you take the medication) include the following:
- q.t.t. means drops
- OD means in the right eye (eye drops)
- OS means in the left eye (eye drops)
- OU means in both eyes (eye drops)
- IM means intramuscularly (muscle injection)
- Subq means subcutaneous (under-the-skin injection)
- IV means intravenous (injection in the vein)
You may see a symbol on your script that looks like a "T" with a dot at the top of it. This abbreviation means one pill. There may be one to 4 Ts with dots at the top of them signifying one to four pills.
Other Prescription Information
Additional details often found in a prescription include whether it can be refilled, and if so, the number of times. It also includes permission for substitutes, if necessary, along with a healthcare provider's signature and the date.
Some prescriptions include "dispense as written," or DAW, in the instructions. This means that no substitute should be used.
Consider a hypothetical prescription for penicillin written as follows:
- Rx Pen VK 250/ml 1 bottle
- iiss ml qid X 7d
Here is what the notation on this prescription means:
- The medication is Penicillin VK and the healthcare provider ordered one 250 milliliter (ml) bottle, which is about 8 ounces.
- The "ii" means 2 and "ss" means 1/2 which translates to 2 1/2 ml, or 1/2 teaspoon.
- The qid X 7d means four times each day for seven days.
Using the information noted on this prescription, the pharmacist will provide a bottle of Penicillin VK with label directions indicating that 1/2 teaspoon of the medication should be taken four times each day for seven days.
As with other medications, your healthcare provider information (name, office address, NPI, etc.) will appear on the penicillin prescription. So will a signature and the date.
Newer Prescriptions Are Often Simpler
In the digital era, prescriptions may be simpler to read. Having a printed prescription means you won't have to try to read or understand your provider's handwriting. Even when the prescription is sent directly to the pharmacy, your provider will give you printed information about your medication and the condition it's used to treat.
Pharmacies, too, have easy-to-read information in plain language. Usually, you can receive these forms when you pick up the drug. If not, ask the pharmacist if you have questions. They are skilled professionals who are well-trained to answer your questions regarding medication dosages, side effects, and adverse effects.
If you don't understand your prescription or the details about it, ask questions. Healthcare providers want you to know what you're taking and why, and feel confident about your treatment.
If you suspect an error on your prescription, notify your healthcare provider and pharmacist right away. Keep an eye on all fields; it's possible to have the right medication but the wrong dosage, for example, or for a provider and pharmacy to miss a potentially serious drug interaction with something you already take.
There's a good chance that your healthcare provider sends prescriptions electronically and directly to the pharmacy, but you may still need to read a prescription yourself. Decoding a prescription is an important skill that can limit any errors and keep you an active partner in your care.
The notations on your prescription are part of a standard format, written in both English and Latin. It includes three basic parts: information about you, information about your provider, and information about the drug they're prescribing and the reason you need it.
Typically, your pharmacist also will provide information about your prescriptions and include printed material that comes with your medications.
Everson J, Cheng AK, Patrick SW, Dusetzina SB. Association of Electronic Prescribing of Controlled Substances With Opioid Prescribing Rates . JAMA Netw Open . 2020 Dec 1;3(12):e2027951. doi:10.1001/jamanetworkopen.2020.27951.
Fallaize R, Dovey G, Woolf S. Prescription legibility: bigger might actually be better . Postgrad Med J . 2018;94(1117):617-620. doi:10.1136/postgradmedj-2018-136010.
Centers for Medicare & Medicaid Services. National Provider Identifier Standard (NPI) .
Drug Enforcement Administration. Prescriptions Q&A .
University of Minnesota. Prescription abbreviations .
Minnesota.gov. Partial list of prescription abbreviations .
American Medical Association. Patient rights .
By Michael Bihari, MD Michael Bihari, MD, is a board-certified pediatrician, health educator, and medical writer, and president emeritus of the Community Health Center of Cape Cod.

Getting clear on the new coding rules can help you eliminate bloated documentation and improve reimbursement to reflect the value of your visits.
THOMAS WEIDA, MD, FAAFP, AND JANE WEIDA, MD, FAAFP
Fam Pract Manag. 2022;29(1):26-31
Author disclosures: no relevant financial relationships.

In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary drivers of visit level selection, rather than the number of history and physical exam bullets.
In this article, we review the context for these changes, describe them briefly, and offer a quick reference tool to help physicians apply the new rules in practice.
The revisions to the E/M outpatient visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements.
Code level selection is now simplified — based on either medical decision making or total time.
The authors' one-page coding reference tool can help simplify the new rules.
HOW WE GOT HERE
In the 2019 Medicare physician fee schedule final rule, released in November 2018, the Centers for Medicare & Medicaid Services (CMS) adopted revisions to the outpatient E/M codes in order to reduce administrative burden. (See https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year .) Originally scheduled for implementation in 2021, these changes would have combined visit levels 2–4 into a blended payment rate (e.g., one rate for 99202-99204 and one rate for 99212-99214), among other changes.
In response, the American Medical Association (AMA) convened a joint CPT Editorial Board and Relative Value Scale Update Committee (RUC) workgroup to build on the changes and propose some alternatives. The workgroup's goals were to decrease administrative burden, payer audits, and unnecessary medical record documentation while ensuring that payment of E/M services is resource-based.
The workgroup approved significant revisions to the outpatient office visit E/M codes. Code 99201 was deleted. The history and/or physical examination and the counting of bullets were eliminated as components for code selection (although history and/or physical examination documentation should still be performed as medically appropriate). Medical decision making (MDM) or time could be used for code level selection. Changes were made to the code descriptors for 99202-99205 and 99211-99215, the definition of medical decision making, and the calculation of time, and a shorter prolonged services add-on code was created. CMS adopted these new E/M coding guidelines. As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M codes. Most of the values increased, yielding an overall increase of more than 10%.
CODING BASED ON MEDICAL DECISION MAKING
For outpatient E/M coding, medical decision making now has three components:
Number and complexity of problems addressed at the encounter,
Amount and/or complexity of data to be reviewed and analyzed,
Risk of complications and/or morbidity or mortality of patient management.
There are four levels of decision making for each of these components: straightforward, low complexity, moderate complexity, and high complexity.
To determine the level of code for a visit, two of the three components must meet or exceed that level of coding. ( See the table .) For example, if the patient has multiple problems addressed at the encounter, but the data is limited and the risk of complications is low, then the level of medical decision making would be low. New patient codes 99202-99205 and established patient codes 99212-99215 use the same components and levels of decision making for code selection.
Determining medical decision making usually starts with identifying the number and complexity of problems addressed and then determining the data or risk components that support that medical decision making. If a second component does not meet or exceed the problem component, then a lower level of decision making is appropriate. The set of tables below illustrate the essential concepts of these code levels. Each level has specific criteria for each component.
Straightforward medical decision making: Codes 99202 and 99212 include one self-limited or minor problem with minimal or no data and minimal risk.
An example of a 99202 or 99212 is an otherwise healthy patient with cough and congestion due to the common cold.
Low complexity medical decision making: Codes 99203 and 99213 include two or more self-limited or minor problems, one stable chronic illness, or one acute uncomplicated illness or injury.
The data component requires one of two categories to establish the level. Category 1 data requires at least two items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, or each unique test ordered. Tests include imaging, laboratory, psychometric, or physiologic data. A clinical lab panel, such as a complete blood count, is a single test. Of note, if a test is ordered, the review of that test is included with the ordering, even if the review is done at a subsequent visit. Tests ordered outside of an encounter may be counted in the encounter in which they are analyzed. Category 2 data includes significant history given by an independent historian. Parents giving the history for their child is a typical example.
The risk component is low. There is low risk of morbidity from additional diagnostic testing or treatment.
An example of a 99203 or 99213 is a sinus infection treated with an antibiotic. Although the prescription makes the risk component moderate, the one acute uncomplicated illness is a low-complexity problem, and there are no data points.
Moderate complexity medical decision making: Codes 99204 and 99214 include two or more stable chronic illnesses, one or more chronic illnesses with exacerbation, progression, or side effects of treatment, one undiagnosed new problem with uncertain prognosis, one acute illness with systemic symptoms, or one acute complicated injury. A patient who is not at a treatment goal, such as a patient with poorly controlled diabetes, is not stable. Systemic general symptoms such as fever or fatigue in a minor illness (e.g., a cold with fever) do not raise the complexity to moderate. More appropriate would be fever with pyelonephritis, pneumonitis, or colitis.
The data component requires one of three categories to establish the level. Category 1 data requires at least three items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, each unique test ordered, or independent historian involvement. Physicians cannot count tests that they or someone of the same specialty and same group practice are interpreting and reporting separately (e.g., electrocardiogram, X-ray, or spirometry). Category 2 data includes the independent interpretation of a test performed by another physician/other qualified health care professional (QHP) (not separately reported). For instance, if a chest X-ray was ordered and the ordering clinician included the interpretation in the visit documentation, this would qualify for data point Category 2. However, if the ordering clinician bills separately for the interpretation of the X-ray, then that cannot be used as an element in this category and would be an element for Category 1. Category 3 data includes discussion of management or test interpretation with an external physician/QHP (not separately reported).
The risk component may include prescription drug management, a decision for minor surgery with patient or procedure risk factors, a decision for elective major surgery without patient or procedure risk factors, or social determinants of health (SDOH) that significantly limit diagnostic or treatment options, such as food or housing insecurity. For prescription drug management, renewing pre-existing chronic medications would qualify. Documentation that the physician is managing the patient for the condition for which the medications are being prescribed would help establish validity in the use of this criterion for MDM.
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. An example using SDOH would be a patient with chronic knee pain and a positive anterior drawer test who needs imaging of the knee but cannot afford this care. Documenting that the patient cannot afford to obtain an MRI of the knee at this time, which significantly limits your ability to confirm the diagnosis and recommend treatment, adds to the risk component.
High complexity medical decision making: Codes 99205 and 99215 include one or more chronic illnesses with a severe exacerbation, progression, or side effects of treatment, or one acute or chronic illness or injury that poses a threat to life or bodily function.
The data component requires two of three categories to establish the level. These data categories are the same as those for 99204 and 99214, and they follow the same rules.
The risk component may include drug therapy requiring intensive monitoring for toxicity. Decisions regarding elective major surgery with patient or procedure risk, emergency major surgery, hospitalization, or “do not resuscitate” orders are also high risk. Intensive prescription drug monitoring is typically supported by a laboratory test, physiologic test, or imaging, and is done to evaluate for complications of the treatment. It may be short-term or long-term. Long-term monitoring is at least quarterly. An example would be monitoring for cytopenia during antineoplastic therapy. Monitoring the therapeutic effect of a treatment, such as glucose monitoring during insulin therapy, is not considered intensive prescription drug monitoring.
An example of a 99205 or 99215 is a patient with severe exacerbation of chronic heart failure who is admitted to the hospital.
CODING OUTPATIENT E/M VISITS
Time-based coding.
An alternative method to determine the appropriate visit level is time-based coding. A major change is that total time now includes both face-to-face and non-face-to-face services personally performed by the physician/QHP on the day of the visit. Additionally, time-based coding is no longer restricted to counseling services. Instead, it includes the following:
Preparing to see the patient (e.g., reviewing external test results),
Obtaining and/or reviewing separately obtained history,
Performing a medically appropriate examination and/or evaluation,
Counseling and educating the patient, family, or caregiver,
Ordering medications, tests, or procedures,
Referring and communicating with other health care professionals (when not separately reported),
Documenting clinical information in the electronic or other health record,
Independently interpreting results (not separately reported with a CPT code) and communicating results to the patient, family, or caregiver.
Care coordination (not separately reported with a CPT code).
Time spent by clinical staff cannot count toward total time. However, time spent by another physician/QHP (not a resident physician) in the same group can be included. If a nurse practitioner performs the initial intake and the physician provides the assessment and plan, both of those times can be counted, although only one person's time can be counted while they are discussing the case with each other. The visit should be billed under the clinician who provided the substantive portion (more than half) of the time, although both clinicians need to be identified in the medical record. Time spent must be documented in the note. It is advisable to specifically document the time spent and the activities performed both face-to-face and non-face-to-face.
The amount of total time required for each level of coding changed under the new time-based coding guidelines. (See the “Total time ” table.)
PROLONGED VISIT CODES
When time on the date of service extends beyond the times for codes 99205 or 99215, prolonged visit codes can be used. The AMA CPT committee developed code 99417 for prolonged visits, and Medicare developed code G2212. These are added in 15-minute increments in addition to codes 99205 or 99215. Code G2212 can be added once the maximum time for 99205 or 99215 has been surpassed by a full 15 minutes, whereas code 99417 can be added once the minimum time for 99205 or 99215 has been surpassed by a full 15 minutes. Less than 15 minutes is not reportable. Multiple units can be reported. Prolonged visit codes cannot be used with the shorter E/M levels, i.e., 99202-99204 and 99212-99214. (See “Prolonged services ” tables.) Clinicians should consult with individual payers to determine which code to use — G2212 or 99417.
SIMPLIFIED CODING AND DOCUMENTATION
The revisions to the outpatient E/M visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements. Only medically appropriate documentation is required. Code level selection is simplified — based on either medical decision making or total time. By applying these changes, primary care clinicians can eliminate bloated documentation and improve reimbursement reflecting the value of the visit.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
BREAKING: Sean 'Diddy' Combs has been arrested
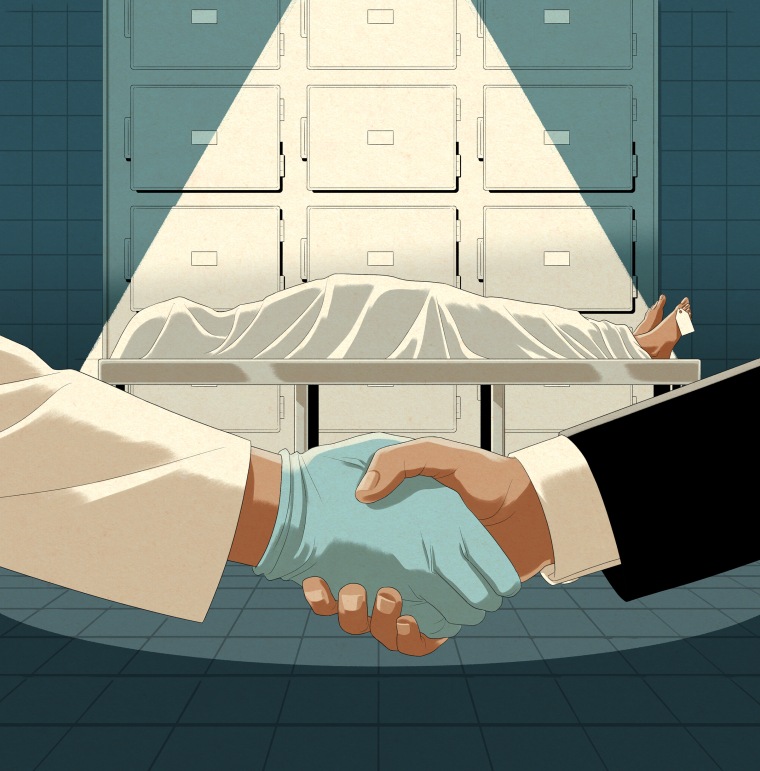
Cut up and leased out, the bodies of the poor suffer a final indignity in Texas
The University of North Texas Health Science Center built a flourishing business using hundreds of unclaimed corpses. It suspended the program after NBC News exposed failures to treat the dead and their families with respect.
DALLAS — Long before his bleak final years, when he struggled with mental illness and lived mostly on the streets, Victor Carl Honey joined the Army, serving honorably for nearly a decade. And so, when his heart gave out and he died alone 30 years later, he was entitled to a burial with military honors.
Instead, without his consent or his family’s knowledge, the Dallas County Medical Examiner’s Office gave his body to a state medical school, where it was frozen, cut into pieces and leased out across the country.
A Swedish medical device maker paid $341 for access to Honey’s severed right leg to train clinicians to harvest veins using its surgical tool. A medical education company spent $900 to send his torso to Pittsburgh so trainees could practice implanting a spine stimulator. And the U.S. Army paid $210 to use a pair of bones from his skull to educate military medical personnel at a hospital near San Antonio.
In the name of scientific advancement, clinical education and fiscal expediency, the bodies of the destitute in the Dallas-Fort Worth region have been routinely collected from hospital beds, nursing homes and homeless encampments and used for training or research without their consent — and often without the approval of any survivors, an NBC News investigation found.

Honey, who died in September 2022, is one of about 2,350 people whose unclaimed bodies have been given to the Fort Worth-based University of North Texas Health Science Center since 2019 under agreements with Dallas and Tarrant counties . Among these, more than 830 bodies were selected by the center for dissection and study. After the medical school and other groups were finished, the bodies were cremated and, in most cases, interred at area cemeteries or scattered at sea. Some had families who were looking for them.
For months as NBC News reported this article, Health Science Center officials defended their practices, arguing that using unclaimed bodies was essential for training future doctors. But on Friday, after reporters shared detailed findings of this investigation, the center announced it was immediately suspending its body donation program and firing the officials who led it. The center said it was also hiring a consulting firm to investigate the program’s operations.
“As a result of the information brought to light through your inquiries, it has become clear that failures existed in the management and oversight of The University of North Texas Health Science Center’s Willed Body Program,” the statement said. “The program has fallen short of the standards of respect, care and professionalism that we demand.”
Last year, NBC News revealed in its “Lost Rites” investigation that coroners and medical examiners in Mississippi and nationally had repeatedly failed to notify families of their loved ones’ deaths before burying them in pauper’s graveyards . That investigation led reporters to North Texas, where officials had come to view the unclaimed dead not as a costly burden, but as a free resource.
Before its sudden shuttering last week, the Health Science Center’s body business flourished.
On paper, the arrangements with Dallas and Tarrant counties offered a pragmatic solution to an expensive problem: Local medical examiners and coroners nationwide bear the considerable costs of burying or cremating tens of thousands of unclaimed bodies each year. Disproportionately Black, male, mentally ill and homeless, these are individuals whose family members often cannot be easily reached, or whose relatives cannot or will not pay for cremation or burial.
The University of North Texas Health Science Center used some of these bodies to teach medical students. Others, like Honey’s, were parceled out to for-profit medical training and technology companies — including industry giants like Johnson & Johnson, Boston Scientific and Medtronic — that rely on human remains to develop products and teach doctors how to use them. The Health Science Center advertised the bodies as being of “the highest quality found anywhere in the U.S.”
Do you have a story to share about the use of unclaimed bodies for research? Contact us .
Proponents say using unclaimed bodies transforms a tragic situation into one of hope and service, providing a steady supply of human specimens needed to educate doctors and advance medical research. But for families who later discover their missing relatives were dissected and studied, the news is haunting, compounding their grief and depriving them of the opportunity to mourn.
“The county and the medical school are doing this because it saves them money, but that doesn’t make it right,” said Thomas Champney, an anatomy professor at the University of Miami Miller School of Medicine who researches the ethical use of human bodies . “Since these individuals did not consent, they should not be used in any form or fashion.”

A half-century ago, it was common for U.S. medical schools to use unclaimed bodies, and doing so remains legal in most of the country, including Texas. Many programs have halted the practice in recent years, though, and some states, including Hawaii, Minnesota and Vermont, have flatly prohibited it — part of an evolution of medical ethics that has called on anatomists to treat human specimens with the same dignity shown to living patients.
The University of North Texas Health Science Center charged in the opposite direction.
Through public records requests, NBC News obtained thousands of pages of government records and data documenting the acquisition, dissection and distribution of unclaimed bodies by the center over a five-year period.
An analysis of the material reveals repeated failures by death investigators in Dallas and Tarrant counties — and by the center — to contact family members who were reachable before declaring a body unclaimed. Reporters examined dozens of cases and identified 12 in which families learned weeks, months or years later that a relative had been provided to the medical school, leaving many survivors angry and traumatized.
Five of those families found out what happened from NBC News. Reporters used public records databases, ancestry websites and social media searches to locate and reach them within just a few days, even though county and center officials said they had been unable to find any survivors.
In one case, a man learned of his stepmother’s death and transfer to the center after a real estate agent called about selling her house. In another, Dallas County marked a man’s body as unclaimed and gave it to the Health Science Center, even as his loved ones filed a missing person report and actively searched for him.
From 2023: NBC News’ “Lost Rites” investigation
- After a mother in Jackson, Mississippi, reported her son missing, police kept the truth from her for months.
- ‘They just threw him away’: Another Mississippi man was buried without his family’s knowledge .
- America’s patchwork death notification system routinely leaves families in the dark.
- The Department of Justice took action after a Mississippi coroner buried men without notifying their families.
- The Jackson Police Department adopted a next-of-kin notification policy following NBC News’ reporting.
Before the Health Science Center announced it was suspending the program, officials in the two counties had already told NBC News they were reconsidering their unclaimed body agreements in light of the reporters’ findings.
Commissioners in Dallas County recently postponed a vote on whether to extend their contract. The top elected official in Tarrant County, Judge Tim O’Hare — who voted to renew the county’s agreement with the center in January — said he planned to explore legal options “to end any and all immoral, unethical, and irresponsible practices stemming from this program.”
“No individual’s remains should be used for medical research, nor sold for profit, without their pre-death consent, or the consent of their next of kin,” O’Hare’s office said . “The idea that families may be unaware that their loved ones’ remains are being used for research without consent is disturbing, to say the least.”
NBC News also shared its findings with dozens of companies, teaching hospitals and medical schools that have relied on the Health Science Center to supply human specimens. Ten said they did not know the center had provided them with unclaimed bodies. Some, including Medtronic, said they had internal policies requiring consent from the deceased or their legal surrogate.
DePuy Synthes, a Johnson & Johnson company, said it had paused its relationship with the center after learning from a reporter that it had received body parts from four unclaimed people. And Boston Scientific, whose company Relievant Medsystems used the torsos of more than two dozen unclaimed bodies for training on a surgical tool , said it was reviewing its transactions with the center, adding that it had believed the program obtained consent from donors or families.
“We empathize with the families who were not reached as part of this process,” the company said.
The Army said it, too, was examining its reliance on the center and planned to review and clarify internal policies on the use of unclaimed bodies. Under federal contracts totaling about $345,000, the center has provided the Army with dozens of whole bodies, heads and skull bones since 2021 — including at least 21 unclaimed bodies. An Army spokesperson said officials had not considered the possibility that the program hadn’t gotten consent from donors or their families.
The Texas Funeral Service Commission, which regulates body donation programs in the state, is conducting a review of its own. In April, the agency issued a moratorium on out-of-state shipments while it studies a range of issues, including the use of unclaimed bodies by the Health Science Center.
In the case of Victor Honey, it shouldn’t have been hard for Dallas County investigators to find survivors: His son shares his father’s first and last name and lives in the Dallas area. Family members are outraged that no one from the county or the Health Science Center informed them of Honey’s death, much less sought permission to dissect his body and distribute it for training.
It wasn’t until a year and a half after he died that his relatives finally learned that news — from a chance encounter with a stranger struck by the similarity of the father’s and son’s names, followed by a phone call from NBC News.
“It’s like a hole in your soul that can never be filled,” said Brenda Cloud, one of Honey’s sisters. “We feel violated.”

Two years before Honey’s death, Oscar Fitzgerald died of a drug overdose outside a Fort Worth convenience store. County officials failed to reach his siblings or adult children, so they had no voice in deciding whether to donate his body. It was taken to the University of North Texas Health Science Center, pumped with preservatives and assigned to a first-year medical student to study over the coming year.
Five months passed before his family learned from a friend in September 2020 that he was dead. When his brother rushed to Fort Worth to claim the remains, he said he was told by the Health Science Center that he’d have to wait — the program was not done using the body.
Patrick Fitzgerald, who had last seen his 57-year-old brother the previous Thanksgiving, was aghast.
“Now that the family has come forward,” he said, “you mean to tell me we can’t have him?”
Instead, Fitzgerald said he was told his family must fill out donation consent forms to eventually receive his brother’s ashes. A year and a half later — after the body had been leased out a second time, to a Texas dental school — the center billed the family $54.50 in shipping costs for the box that arrived at Fitzgerald’s Arkansas home containing his brother’s remains. He also received a letter from Claudia Yellott, then the manager of UNT’s body donation program.
“UNT Health Science Center and our students value the selfless sacrifice made by your family,” Yellott wrote.
As of Friday, Yellott’s photo and bio were missing from the Health Science Center website, along with those of Rustin Reeves, the longtime director of the center’s anatomy program . Yellott confirmed to NBC News that she had been terminated and declined to comment further. Reeves did not respond to messages. The center declined to specify who was fired.
The Fitzgeralds’ ordeal was the scenario one Tarrant County commissioner had feared in 2018, when Yellott and Reeves pitched their plan to receive the county’s unclaimed dead.
They described it as a win for everyone: The county would save on burial costs and the center would, as Yellott phrased it , obtain “valuable material” needed to educate future physicians.
The commissioners were elated at the prospect of saving up to a half-million dollars a year. But one, Andy Nguyen, questioned the morality of dissecting bodies of people with no family to consent and raised the possibility of survivors coming forward later, horrified to learn how their relatives were treated.
“Just because they don’t have any next of kin doesn’t mean they have no voice,” Nguyen said .
After the Health Science Center pledged to handle each body with dignity, all five commissioners voted to approve the agreement. A little over a year later, Dallas County struck a similar deal, with one major difference: While Tarrant County families who couldn’t afford to make funeral arrangements were given an option to donate their relatives’ bodies to the center, Dallas County gave survivors no choice.
Soon, a steady stream of bodies began to flow to the center. The program went from receiving 439 bodies in the 2019 fiscal year to nearly 1,400 in 2021 — about a third of them unclaimed dead from Dallas and Tarrant counties. This coincided with a multimillion-dollar expansion and renovation of the Health Science Center’s body storage facilities and laboratories.
The supply of unclaimed dead helped bring in about $2.5 million a year from outside groups, according to financial records . Many of those payments came from medical device makers that spent tens of thousands of dollars to use the center-run laboratory space, BioSkills of North Texas, to train clinicians on how to use their products — a revenue stream made possible by the school’s robust supply of “cadaveric specimens.”
That economic engine has now stalled; the center announced it was permanently closing the BioSkills lab in response to NBC News’ findings. In its statement, the center said it “is committed to addressing all issues and taking corrective actions to maintain public trust.”
The partnerships with Dallas and Tarrant counties, which drew little attention when they were adopted, quietly rippled through the community of professionals who work with the dead and dying in North Texas.
Eli Shupe, a bioethicist at the University of Texas at Arlington, was volunteering with a Tarrant County hospice provider in late 2021 when a chaplain made a comment that rocked her.
“Oh, poor Mr. Smith,” Shupe recalled the chaplain saying. “He doesn’t have long, and then it’s off to the medical school.”

Her shock led Shupe to spend months studying the use of unclaimed bodies in Texas. As she investigated, she pondered a philosophical question: People have the right to make decisions about their bodies while they’re alive, but should that right die with them?
No, she ultimately concluded, it should not.
Shupe herself has signed up to give her body to the Health Science Center when she dies, in part to underscore that she doesn’t oppose body donation. But she emphasized that it was her choice.
“What they’re doing is uncomfortably close to grave-robbing,” she said.
Shupe was alluding to the dark history, long before voluntary body-donation programs, when U.S. medical schools turned to “resurrectionists,” or “body snatchers,” who dug up the graves of poor and formerly enslaved people. To curb this ghastly 19th-century practice, states adopted laws giving schools authority to use unclaimed bodies for student training and experiments.
Many of those laws remain on the books, but the medical community has largely moved beyond them. Last year, the American Association for Anatomy released guidelines for human body donation stating that “programs should not accept unclaimed or unidentified individuals into their programs as a matter of justice.”
Experts said the Health Science Center appeared to be an outlier in terms of the number of unclaimed bodies it used. No national data exists on this issue, so NBC News surveyed more than 50 major U.S. medical schools. Each of the 44 that answered said they don’t use unclaimed bodies — and some condemned doing so.
Joy Balta, an anatomist who runs a body donation program at Point Loma Nazarene University, chaired the committee that wrote the anatomy association’s new guidelines. He said using unclaimed bodies violates basic principles of dignity and consent now embraced by most experts in his field.
One reason that bodies should come only from consenting donors, Balta and others note: Some religions have strict views about how the dead should be treated.
“We don’t know if the individual is completely against their body being donated, and we can’t just disregard that,” Balta said.
Since 2021, dozens of entities have received unclaimed bodies from the Health Science Center — including some, like the University of Arkansas for Medical Sciences, that explicitly prohibit the practice on ethical grounds.
The Little Rock-based school received shipments of skull bones and heads in 2023 and 2024 that included parts harvested from unclaimed bodies, records show. Leslie Taylor, a University of Arkansas medical school spokesperson, said because the UNT office that provided specimens is called the Willed Body Program , officials “believed they came from donors who willed their remains for education and study.”
Taylor said the school would adopt procedures to ensure it receives bodies only from people who have given explicit permission.
Before abruptly suspending the program last week, the Health Science Center had vigorously defended its practices.
“An unclaimed individual is incapable of consenting to any process after death, which includes burial, donation, cremation, eco-burials or any other use of the body,” the center had said in a statement on Aug. 16. “If a relative is not located or does not claim the remains, a decision must still be made.”
Shupe argued that it’s problematic for a public medical school to benefit from the deaths of the “very poor” in its community. She has now embarked on a campaign to end the use of unclaimed bodies in Texas and nationally.
After publishing a newspaper essay criticizing the practice, she brought her concerns directly to the Tarrant County Commissioners Court at a meeting last year, asking officials to consider the message being sent to marginalized residents and people of color.
“How does it look,” she said , “when a Black body is dissected with nobody’s permission at all, simply because they died poor?”
All Victor Honey’s family has to go by are faded memories, a handful of keepsakes, online snapshots and a trail of court records spanning eight states and Washington, D.C. These clues tell a disjointed story of an Army veteran tormented by paranoid delusions who repeatedly rejected help as he slid into homelessness and whose body went unclaimed, despite having a family who cared deeply for him.
His two sisters remember Honey teaching them math, making them laugh, shielding them from bullies and helping raise them when their parents divorced and moved the family from Mississippi to Cleveland in the 1970s. He was meticulous, hardworking, well-dressed — and in search of a calling.
After starting college, Honey joined the Army in late 1984 and reported to Texas’ Fort Hood, where he trained as a medic and, at a military club, danced with a soon-to-be Air Force enlistee named Kimberly. They married not long after and had a daughter. A son followed.
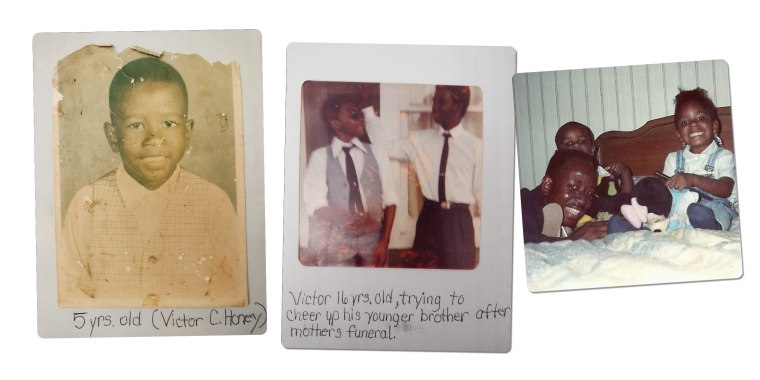
The young family lived at the base until 1988, when Honey’s enlistment ended. He then joined the Army Reserves in Dallas and was called up to support the first Gulf War. Though he didn’t want to go, he spent four months in Germany, so upset about the deployment that he rarely left his base. He remained angry after he returned home.
Kimberly Patman said Honey had multiple affairs, leading them to separate in 1992, which threw him into a deep depression. He sought mental health services from a local Department of Veterans Affairs facility and was given antipsychotic medication that he quit after a month, saying he was allergic.
From there, his life unraveled.
In 1995, Honey was arrested in Dallas for trespassing. A doctor at the jail called Patman and said he’d had some kind of breakdown. She called his father in Cleveland, who brought him home.
He was diagnosed with paranoid schizophrenia but refused to take the medication that eased his delusional thoughts. He was convinced people were coming after him, barricaded himself in his room and became a compulsive hoarder, filing papers in a leather satchel.
He was off his medications in early 1997 when he stole a car from a dealership and robbed three banks in three states — each time handing a teller a note demanding money. He had no weapon. He was sentenced to three years in federal prison.
After he was released, Honey tried living in Cleveland, but abruptly left.
“He just disappeared,” Patman said. “They didn’t know where he was. We didn’t know where he was. And it was like that for years.”
He eventually drifted to Washington, where he wound up on the streets. He filed more than a dozen lawsuits, claiming an array of grievances. He posted a video to YouTube in which he showed his broken teeth and suggested the police were responsible. “This is a horrendous, horrendous life here in Washington,” he told the camera.
He landed in Dallas again in late 2018. He was arrested multiple times for fare evasion and filing a false police report, and appeared at city council meetings claiming he’d been wrongfully charged. He also pleaded guilty to assaulting an emergency room nurse who was attempting to provide him care.
And then came the phone call that brought the family together again.

In early 2022, a caseworker at a Dallas-area hospital contacted Honey’s daughter, Victoria, in Montgomery, Alabama, to say he was in intensive care and might not survive, the family said. Patman and Victoria rushed to his side and were told his kidneys were failing.
“We’re here, the kids are here, we love you,” Patman told Honey. In response, he opened his eyes and asked, “Why did you divorce me?” They ended up laughing about it.
Brenda Cloud, his sister, called from Cleveland. “I would just talk to him and remind him of growing up and of his children, and he had a lot to fight for,” she said.
Honey’s condition improved, but he ignored advice to go to a nursing home and instead checked himself out. Several weeks later, he got on the phone with his namesake son. They’d often gone years without talking, but the son said he knew his father loved him.
That was Victor Carl Honey’s last contact with his family.
On Sept. 19, 2022, Honey was discovered semiconscious in a wheelchair at a downtown Dallas light rail station and taken to Baylor University Medical Center. He died early the next morning. He was 58.

After a Baylor social worker was unable to find his family, Honey’s body was transported to the Dallas County Medical Examiner’s Office, where an investigator was assigned to find next of kin.
The county investigator sought information from police and area hospitals but was unable to locate relatives. She then turned to the internet, where she found numbers for Patman, Honey’s brother in Ohio, his stepmother and his late father, but she reported they were disconnected. On Oct. 17, 2022, the investigator wrote that her search was complete and no family was found. The medical examiner’s office deemed Honey’s body unclaimed.
That same day, Honey was delivered to the University of North Texas Health Science Center, where he was placed in a freezer, awaiting assignment.
One of the most solemn duties of local government is notifying families when someone dies. Though the world, in so many ways, has never been more connected, finding survivors still can be difficult in an era of growing homelessness and increasingly fractured families.
Death investigators at the Dallas County Medical Examiner’s Office follow a detailed checklist: They reach out to area hospitals to seek emergency contact information, search missing person reports, and comb public records databases for possible phone numbers. They also call neighbors and homeless shelters. If no family is found, they must sign an affidavit stating they did all they could.
In Tarrant County, officials delegated the primary responsibility for contacting next of kin to the Health Science Center, which said it takes similar steps.
But these efforts repeatedly fell short.
For two and a half years, Fran Moore of Lodi, New York, didn’t know what happened to her 79-year-old father, Carl Yenner. She cried when an NBC News reporter notified her in February that he had died at a Dallas hospital in May 2021 and his body had been sent to the Health Science Center.
Moore said she and her brother had struggled to stay in touch with their father across the miles. After not hearing from him, her brother filed a missing person report in Wichita Falls, about two hours from Dallas, where Yenner had lived. They still don’t know how he wound up in Dallas, how he died or why nobody contacted them. A Dallas County worker signed a form in June 2021 stating she had completed an exhaustive search for possible relatives.
But after spotting Yenner’s name on a list of unclaimed bodies provided by Dallas County, NBC News quickly identified Moore and her brother as Yenner’s children and found working phone numbers for each of them.
“If you could find us,” Moore said, “why didn’t they?”
Another question left unanswered: Given that Yenner was an Army veteran and entitled to federal burial benefits , what was the economic argument for Dallas County to send his body to the Health Science Center? At least 32 unclaimed veterans, including Honey, have been given to the program since 2020, records show.
After the center was done with Yenner’s body, it was cremated and interred among fellow service members at Dallas-Fort Worth National Cemetery. Moore said she’s heartbroken she couldn’t bury him with the rest of his family in New Jersey.
“To not have any kind of funeral for him,” she said, “for his family to come see him to say goodbye?”
Without commenting on specific cases, Dallas County Administrator Darryl Martin offered condolences to families whose relatives were used by the program. He said his staff works hard to locate family members and treats bodies with dignity. He didn’t address the use of unclaimed veterans.
In January, in an attempt to improve its efforts to find survivors in Tarrant County, the Health Science Center hired a company called The Voice After Life , whose mission is to help governments locate families of the unclaimed. The center said it has found families in about 80% of cases since then; officials did not know the previous success rate.
In a statement issued weeks before announcing it was suspending the program, the center said it “seeks to understand and honor the wishes of the family and deceased.”
It did not, however, honor the wishes of Michael Dewayne Coleman’s relatives.
Coleman, 43, died alone on Oct. 21, 2023, in a Dallas hospital after possibly being hit by a car. An investigator for the medical examiner signed off on his case file, saying “all reasonable efforts” had been made to find next of kin.
But his relatives should have been easy to reach. More than a week before his death, his fiancée, Louisa Harvey, had filed a missing person report with the Dallas Police Department after he failed to return from a night out with friends, not knowing he was already languishing in a hospital. She spent months searching for him, alongside two of Coleman’s sisters. She printed missing person posters and canvassed neighborhoods near their home.

She said she called the detective assigned to the missing person case almost every day, eventually suspecting that finding Coleman wasn’t a priority because of his criminal record, which included illegal drug use and two domestic violence convictions.
Harvey finally learned of his death in March, after the Dallas County medical examiner listed him as an unclaimed body in the National Missing and Unidentified Persons System, or NamUs , a free federal database meant to connect missing person reports with reports of unclaimed bodies. By the time Harvey found the posting online, the medical examiner had sent Coleman’s body to the Health Science Center.
His family could have learned of his death months earlier if the police detective assigned to find Coleman had listed him as a missing person in NamUs, but records show he never did. In response to questions from NBC News, a Dallas Police spokesperson said the department had opened an internal investigation into the detective’s handling of the case and would implement a policy change to prevent similar mistakes.
Harvey couldn’t believe Coleman’s body had been donated without the family’s consent — or his. Last year, while filling out an application for a state ID, she said, Coleman had made clear he didn’t want his organs donated because of his distrust of the medical system; she doubts he would have wanted to donate his whole body.
But when Harvey and one of Coleman’s sisters, Shea Coleman, repeatedly asked the medical examiner and the Health Science Center to release his body — or at least to let them view it — they were told no. In June, a worker at the medical examiner’s office wrote in case notes that she spoke to Yellott, the manager of UNT’s body donation program, who told her Coleman was slated to be used in a longer-term course and that his family could receive his remains when the center was finished with him.
In 12 to 24 months.
In August, after NBC News inquired about his case, a Health Science Center official told reporters that Coleman’s body would be cremated and returned to the family much sooner — an abrupt reversal that the center attributed to the Texas Funeral Service Commission’s temporary ban on out-of-state body shipments. Ten days later, the medical examiner called Harvey to let her know Coleman’s ashes were ready to be picked up.
The center’s refusal to let her see her fiancé’s body has made it harder to grieve, Harvey said.
“I’m lying awake every night thinking, ‘Is that my Michael?’” she said. “‘Did he actually die?’”
After Victor Honey’s body arrived at the University of North Texas Health Science Center, the harvesting began.
Depending on how they were to be used, bodies were either frozen or embalmed. Some were left whole and set aside to train students. Others, like Honey’s , were dissected with scalpels and bone saws, to be distributed on the open market.
In November 2022, Honey’s right leg was used in a training at the center paid for by Getinge, a Swedish medical technology company that makes instruments for use in a surgical procedure called endoscopic vein harvest.
In January 2023, a week after the medical examiner’s office reported that Honey was eligible for a veteran’s burial, bones from his skull were shipped to Brooke Army Medical Center at Fort Sam Houston — where Honey had been ordered to report before his Gulf War deployment more than three decades earlier.
In May 2023, the Health Science Center shipped Honey’s torso to Pittsburgh, where the training company National Bioskills Laboratories provided it to a medical product company renting its facilities to teach doctors a pain-relief procedure called spinal cord stimulation.
NBC News informed Getinge, the Army and National Bioskills about the center’s regular use of unclaimed bodies and Honey’s family not providing consent.
Dr. Douglas Hampers, National Bioskills’ CEO and an orthopedic surgeon, said he was disturbed to learn his company has received unclaimed bodies and expressed sympathy for Honey’s family.
While human specimens are crucial for medical advances, Hampers said bodies should not be used without consent. He said his company would ensure that it no longer accepted unclaimed bodies and would adopt policies to make certain future specimens were donated with families’ permission.
“I don’t think you have to violate a family’s rights in order to train physicians,” he said.
A Getinge spokesperson emailed a statement saying only that the company regularly reviews its policies and operations, “including what we expect from our suppliers.”
In a statement, the Army said that if Honey’s remains were procured legally, the use of his body complied with the service’s current policies.
In July 2023, after Honey’s torso had been returned to the Health Science Center, his remains were cremated and later his ashes were brought to the Dallas County medical examiner.
And there they sat, with no one to claim them. Months passed.

In late April, Honey’s son, Victor, was boxing cans at the Dallas food bank where he volunteered when a woman approached him. She’d overheard someone calling out his name. “Do you know someone else named Victor Honey?” she asked him.
The woman said she knew his father when they both stayed at a downtown homeless shelter and had heard he died. Victor didn’t want to believe it. He tried to put it out of his mind. But the next morning, he called his mother and told her what he’d heard. She cried out and burst into tears.
An internet search led Victor to the medical examiner’s office, which confirmed the details of his father’s death and later told him the remains were available to be picked up.
About the same time, NBC News had found Honey’s name on a list of people whose unclaimed bodies were obtained by the Health Science Center. Using public records, a reporter tracked down Patman, Honey’s ex-wife, and sent her a message on Facebook. She responded immediately.
On a call, the reporter broke the news of how Honey’s body was used.
His family was appalled. Patman said she would have argued against Honey being cut apart and studied, noting that he once told her that he didn’t want to be an organ donor. Victor, though, said he might have been open to donating his father’s body for medical research.
“But y’all should have asked us about it,” he said. “They just sent his body parts away.”

When the family gathered in early June to finally lay Honey to rest, many expressed remorse about not being able to help him. They were frustrated to have no say in what happened to his body. And they said they hoped sharing his story would help spare others from similar anguish.
“Victor had a big, strong family,” Patman told family members. “And now we are going to speak for him.”
On a muggy Monday morning, a couple dozen of Honey’s relatives — nieces and nephews, siblings and cousins, Patman and their children — gathered in a pavilion at the Dallas-Fort Worth National Cemetery for the farewell they had long been denied.
A recording of taps played. A soldier knelt in front of Honey’s daughter, Victoria, and handed her a folded U.S. flag “as a symbol of our appreciation of your loved one’s honorable and faithful service.”
After the funeral, Honey’s relatives made their way to Section 40, Grave No. 464, where a crew dug a hole and placed the urn in the ground. They installed a temporary marker that soon would be replaced by a white granite headstone standing among rows of thousands.
Brenda Cloud, Honey’s sister, is furious over what transpired in the 622 days between her brother’s death and his burial. And she wants answers for the others whose bodies were cut up and studied without consent.
“Whether they had family or not,” she said, “every person deserves to have that dignity.”

Mike Hixenbaugh is a senior investigative reporter for NBC News, based in Maryland, and author of "They Came for the Schools."
Jon Schuppe is an enterprise reporter for NBC News, based in New York.
Susan Carroll was a senior enterprise editor for NBC News, based in Houston.

IMAGES
VIDEO
COMMENTS
D1 in Medical commonly refers to the first dorsal vertebra, which is the uppermost of the thoracic vertebrae in the spinal column, playing a crucial role in supporting the rib cage and facilitating movement of the upper body. Explore categories such as Anatomy and Physiology for more information. Share. Vote. 2.
D1: If one of the above condition codes does not apply and there is a change to the COVERED charges this code should be used. ... Distinct medical visit. Multiple medical visits/evaluation and management visits occurred on the same day in the same revenue center and the visits were distinct and constituted independent visits. Not reported by CAHs.
Other insurers use CPT code 99417, which is for established patient visits of 55 minutes or more and new patient visits of 75 minutes or more. With both codes, prolonged services are billed in 15 ...
D1. Changes to Charges. Self-explanatory. D2. Changes to Revenue Codes/HCPCS/HIPPS Rate Code. ... Distinct Medical Visit. Report this code when multiple medical visits occurred on the same day in the same revenue center. The visits were distinct and constituted independent visits. An example of such a situation would be a beneficiary going to ...
The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The ...
On Jan. 1, 2021, revised office/outpatient visit E/M CPT® codes (99202-99215) and associated documentation went into effect. The revised codes are the culmination of collaboration among the Centers for Medicare & Medicaid Services, American Medical Association and other medical specialty societies, including IDSA. The changes to these codes were
Condition code D1. Only use when changing total charges. Do not use when adding a modifier; it makes a non-covered charge, covered. Condition code D9. If condition code D9 is the most appropriate condition code to use, please include the change (s) made to the claim in 'remarks'. Below are suggested remarks to include on the adjustment claim.
Whether the patient is new or established, and whether the exam is limited or comprehensive, the history documentation requirements for Eye visit codes will be the same in 2021 as they were in 2020. Increased E/M Payments. Payments for office-based E/M codes—but not for Eye visit codes—are slated for a "significant" increase on Jan. 1 ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
On Jan. 1, 2021, the Evaluation and Management (E/M) Office Visit code changes went into effect. Incorporating these groundbreaking revisions into physician workflows, software, health plans and elsewhere is vital to realizing the benefits of this burden reduction initiative. The AMA and Nordic have collaborated to author three white papers ...
99202 through 99205: Office or other outpatient visits for the evaluation and management of a new patient, with the CPT code differing depending on how long the provider spends with the patient. 93000: Electrocardiogram with at least 12 leads. 36415: Collection of venous blood by venipuncture (drawing blood).
For that under our new 2021 calculation, it is going to be based just on total visit time on the day of the patient encounter. So much, much simpler in the office and outpatient world. Stephani: Okay. Thank you. So Elizabeth, tell us exactly how this new total visit time is defined and what activities can be counted towards that total time.
CPT Coding Guidelines for Office Visits. December, 1998. Documentation in the clinical record must support the level of service as coded and billed. The Key Components - History, Examination, and Medical Decision Making - must be considered in determining the appropriate code (level of service) to be assigned for a given visit.
D1 Claim/service denied. Level of subluxation is missing or inadequate. D2 Claim lacks the name, strength, and dosage of the drug furnished. D3 Claim/service denied because information to indicate if the patient owns the equipment that requires the part or supply was missing. D4 Claim/service does not indicate the period of time for which this ...
Clinic or emergency department visit: Paid under OPPS; separate APC payment. X: Ancillary service: Paid under OPPS; separate APC payment. Y: Non-implantable Durable Medical Equipment (DME) Not paid under OPPS. All institutional providers other than home health agencies bill to DME MAC. Resources. CMS Addendum A and Addendum B Updates .
The national average for family physicians' usage of the level 4 code (99214) is slowly increasing and is approaching 50% of established patient office visits (it's now above 50% for our Medicare ...
A single specialty group (193400000X) is a business group of one or more individual practitioners, all of who practice within the same area of specialization. Single specialty groups will normally reflect the actual area of specialization code rather than the 193400000X code. CMS. SPECIALTY CODE. CMS SPECIALTY DESCRIPTION. PROVIDER TAXONOMY CODE.
289 Background: One of the more challenging aspects of managing patients receiving chemotherapy is to reduce Emergency Room (ER) visits and ultimately hospital readmissions. Patients may not understand who or when to call with issues and may be concerned about reaching their physician or receiving a call back in a reasonable amount of time. Methods: C1/D1 calls were initiated with the Medical ...
A prescription will always identify the healthcare provider who ordered the medication and the person who needs it. Your first and last name, along with a date of birth, are displayed. Some states require an address. Some of the provider's information will be obvious to you, such as the name and office you visit.
Addendum D1.—. Payment Status Indicators. Not paid under OPPS. Paid by fiscal intermediaries under a fee schedule or payment system other than OPPS. Not paid under OPPS. Paid by fiscal intermediaries under a fee schedule or payment system other than OPPS. Ambulance Services. Not paid under OPPS.
These two questions can guide you through the coding of many visits: 1. Did you spend 30 minutes (for an established patient) or more of total time on the visit that day? If you did, and you ...
*****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collecti on burden approved under the associated OMB control number listed on this form
A Texas medical center has been studying and leasing out the body parts of unclaimed people without the consent of that person or any survivors. After an NBC News investigation exposed its ...
In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary ...
The medical examiner's office deemed Honey's body unclaimed. That same day, Honey was delivered to the University of North Texas Health Science Center, where he was placed in a freezer ...