- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Wandering Atrial Pacemaker
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Key features, clinical presentation, diagnostic evaluation, ongoing management.
- Full Chapter
- Supplementary Content
ESSENTIALS OF DIAGNOSIS
Progressive cyclic variation in P-wave morphology
Heart rate 60–100 bpm
Variation of P-wave morphology, P-P interval, and P-R interval
GENERAL CONSIDERATIONS
This rhythm is benign
This rhythm and multifocal atrial tachycardia are similar except for heart rate
The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity
Usually, it is associated with underlying lung disease
In the elderly, it may be a manifestation of sick sinus syndrome
In the young and athletic heart, it may represent enhanced vagal tone
SYMPTOMS AND SIGNS
Usually causes no symptoms and is incidentally discovered
Occasional patient may feel skipped beats
PHYSICAL EXAM FINDINGS
Variable S 1
DIFFERENTIAL DIAGNOSIS
Multifocal atrial tachycardia (heart rate > 100 bpm)
Frequent premature atrial complexes and atrial bigeminy
LABORATORY TESTS
None specific
ELECTROCARDIOGRAPHY
ECG to document rhythm
CARDIOLOGY REFERRAL
Not required
MEDICATIONS
No specific treatment
Monitor and treat the underlying cause, such as sick sinus syndrome or lung disease
DIET AND ACTIVITY
No restrictions
General healthy lifestyle
Once a year if sinus node abnormality is suspected; otherwise when symptoms arise
COMPLICATIONS
May progress to sick sinus syndrome
This condition by itself is benign
PRACTICE GUIDELINES
Indications for pacemaker:
– If part of sick sinus syndrome
– If associated with documented symptomatic bradycardia
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Website maintenance is scheduled for Saturday, September 7, and Sunday, September 8. Short disruptions may occur during these days.

A. KESH HEBBAR, M.D., AND WILLIAM J. HUESTON, M.D.
A more recent article on common types of supraventricular tachycardia is available.
Am Fam Physician. 2002;65(12):2479-2487
This is part I of a two-part article on common arrhythmias. Part II, “Ventricular Arrhythmias and Arrhythmias in Special Populations,” appears on page 2491 of this issue.
Family physicians frequently encounter patients with symptoms that could be related to cardiac arrhythmias, most commonly atrial fibrillation or supraventricular tachycardias. The initial management of atrial fibrillation includes ventricular rate control to provide adequate cardiac output. In patients with severely depressed cardiac output and recent-onset atrial fibrillation, immediate electrical cardioversion is the treatment of choice. Hemodynamically stable patients with atrial fibrillation for more than two days or for an unknown period should be assessed for the presence of atrial thrombi. If thrombi are detected on transesophageal echocardiography, anticoagulation with warfarin for a minimum of 21 days is recommended before electrical cardioversion is attempted. Patients with other supraventricular arrhythmias may be treated with adenosine, a calcium channel blocker, or a short-acting beta blocker to disrupt reentrant pathways. When initial medications are ineffective, radiofrequency ablation of ectopic sites is an increasingly popular treatment option.
Heart palpitations and cardiac arrhythmias are common problems encountered by family physicians. Patients may present with acute cardiac rhythm abnormalities. Although these arrhythmias are usually benign, they can indicate significant underlying heart disease. More often, patients have chronic arrhythmias, such as atrial fibrillation, that may require treatment to reduce the risk of future complications. The challenges for the family physician are to determine which arrhythmias are benign and which indicate probable cardiac malfunction, and to manage recurrent or chronic rhythm abnormalities.
This two-part article reviews common atrial and ventricular arrhythmias, with a focus on initial management decisions. Part I discusses supraventricular arrhythmias. Part II discusses ventricular arrhythmias and the management of rhythm abnormalities in special populations, including pregnant women, athletes, and children.
Atrial Fibrillation
Atrial fibrillation is the most common cardiac arrhythmia family physicians are likely to encounter. This rhythm abnormality affects 3 to 5 percent of patients more than 60 years of age 1 and becomes increasingly common with advancing age. The median age of patients with atrial fibrillation is 75 years, and the prevalence of the arrhythmia doubles every 10 years after the age of 55. 2 , 3 In the United States, atrial fibrillation is estimated to affect almost 9 percent of patients more than 75 years of age. 2
Most risk factors for atrial fibrillation are associated with structural or ischemic heart disease. Risk factors include hypertension, left ventricular hypertrophy, dilated and restrictive cardiomyopathies, coronary artery disease, chronic obstructive pulmonary disease, and diabetes in women. 1
The annual risk of stroke in patients with atrial fibrillation and normal valve function has been reported to be 4.5 percent per year. 4 Anticoagulation with warfarin (Coumadin) reduces the risk by about two thirds. 4 The mortality rate for stroke in patients with atrial fibrillation is approximately twice as high as the rate in patients without this rhythm abnormality. 5 Although anticoagulation is contraindicated in some elderly patients, a study in Great Britain 6 found that about 60 percent of patients identified in community screenings as having atrial fibrillation were eligible for, and would benefit from, this treatment.
The first step in managing a patient with atrial fibrillation is to decide whether there is a high likelihood of safe conversion to sinus rhythm or whether the patient should be allowed to remain in atrial fibrillation. A patient with recent onset of atrial fibrillation (within the previous 12 months) and no evidence of enlargement of the left atrium has a greater chance of achieving and maintaining sinus rhythm. If the arrhythmia is long-standing and the patient is not a suitable candidate for rate cardioversion, initial treatment should focus on ventricular rate control, with consideration given to long-term stroke prophylaxis.
Restoration of Sinus Rhythm
Patients who present within 48 hours of the onset of new atrial fibrillation are candidates for cardioversion with a low risk of embolism. Conversion to sinus rhythm can be attempted by electrical shock or with antiarrhythmic drugs. Patients who have been in atrial fibrillation for more than 48 hours or for an undetermined period are more likely to have atrial thrombi and may develop emboli with immediate electrical or medical (pharmacologic) cardioversion.
Atrial thrombi are not evident on transthoracic echocardiograms, but they can been seen on transesophageal echocardiograms. 7 If the transesophageal echocardiogram reveals thrombi, anticoagulation is recommended before cardioversion is attempted. Anticoagulation can be accomplished using warfarin, with the dosage adjusted to achieve an International Normalized Ratio (INR) between 2.0 and 3.0 for a minimum of 21 days. 8
If the transesophageal echocardiogram does not show thrombi on multiplane views, cardioversion can be attempted. Short-term anticoagulation with heparin should be started before the procedure, and warfarin therapy should be initiated after cardioversion. 8
When rhythm conversion is indicated, it can be accomplished using direct-current cardioversion or pharmacologic therapy. Synchronized cardioversion is currently considered the treatment of choice for the restoration of sinus rhythm and, in appropriately selected patients, has a success rate of at least 80 percent. 4 Cardioversion is also indicated in patients with hypotension, angina, heart failure, or other evidence of severe compromise caused by atrial fibrillation. 5
Medical cardioversion of atrial fibrillation may be achieved with class IA drugs (quinidine, disopyramide [Norpace], procainamide [Procanbid]) or with amiodarone (Cordarone). In the past, quinidine was frequently used for both cardioversion and maintenance of sinus rhythm in patients who had undergone electrical cardioversion. However, because of the proarrhythmic action of class IA agents and their detrimental effects on left ventricular function, these drugs are now used less often than amiodarone for primary therapy of atrial fibrillation. 4
Amiodarone therapy is successful in 86 percent of patients who have had atrial fibrillation for less than two years. 4 , 9 Treatment is also effective in 40 to 60 percent of patients with long-standing atrial fibrillation that has been resistant to other agents and to electrical cardioversion. 4 Amiodarone can be given in a dosage of 200 mg a day, which is lower than the dosages that have been associated with thyroid abnormalities and pulmonary fibrosis. Although there is little risk of toxicity when amiodarone is given in a low dosage, it is prudent to monitor patients for the development of thyroid, pulmonary, hepatic, and cardiac side effects.
Findings on the usefulness of various agents for the conversion of atrial fibrillation, based on the evidence-based practice program of the Agency for Healthcare Research and Quality, are summarized in Table 1 . 10 Although drugs such as digitalis preparations and sotalol (Betapace) are sometimes used for rate control, they are not effective for converting atrial fibrillation to sinus rhythm. 10 , 11
If external electrical cardioversion is unsuccessful and antiarrhythmic drug therapy fails, other measures can be used. However, these approaches are usually reserved for use in patients who cannot tolerate atrial fibrillation and patients who have associated systolic dysfunction. Techniques include internal electrical cardioversion through the application of electrical current to pulmonary veins via a transcatheter cathode 4 and radiofrequency ablation of the atrioventricular node with insertion of a ventricular pacemaker. 12 In addition, an implantable atrial defibrillator can be used to provide rapid cardioversion in patients with atrial fibrillation that cannot be controlled with medications. 13
Rate Control in Chronic Atrial Fibrillation
In patients in whom rhythm conversion is not indicated or those who have new-onset atrial fibrillation with a rapid ventricular response, treatment may be needed to control the ventricular rhythm. Excessive ventricular rates may result in diminished cardiac output because of poor filling time, and in ischemia because of increased myocardial oxygen demand. Medications used for ventricular rate control in patients with atrial fibrillation are listed in Table 2 . 14
Acute management of ventricular rates can usually be achieved with intravenously administered diltiazem (Cardizem), given in an initial bolus of 15 to 20 mg (0.25 mg per kg) over two minutes, or with an intravenously administered beta blocker such as propranolol (Inderal), given in a dose of 0.5 to 1 mg (up to 3 to 5 mg if needed).
A number of medications, including calcium channel blockers, beta blockers, and digoxin (Lanoxin), are effective for maintaining ventricular rates within acceptable ranges. Because calcium channel blockers are associated with better exercise tolerance, they may be preferable to beta blockers. 15 Digoxin is associated with a high degree of exercise intolerance; therefore, it should be reserved for use in patients who are relatively immobile, who cannot tolerate other treatment options, or who have significant ventricular dysfunction.
Paroxysmal Supraventricular Tachycardias
Based on duration, supraventricular tachycardias are usually categorized as paroxysmal, persistent, or chronic. Paroxysmal supraventricular tachycardia (PSVT) is the most common of these arrhythmias and the one that is most often encountered in the primary care setting. Longer-duration supraventricular tachycardias can be treated similarly to PSVT, but cardiology consultation is often required to identify the electrophysiologic mechanism responsible for sustaining the arrhythmia. In contrast to ventricular tachycardias (discussed in part II of this article) and atrial fibrillation, PSVT is usually a narrow-complex tachycardia with a regular rate.
Atrioventricular Nodal Reentry Causing PSVT
Atrioventricular nodal reentry, the most common mechanism of PSVT, occurs when two pathways exist with different conduction rates. A premature atrial complex that is blocked in the fast pathway and redirected through the slow pathway usually triggers the tachycardia ( Figure 1 ) . The electrical signal proceeds down the slow pathway and then reenters the fast pathway in a retrograde direction. By the time the signal has propagated down the slow pathway and back around on the fast pathway, the slow pathway is no longer refractory and is ready to conduct the signal again, completing a continuous circuit.
Reentrant tachycardias usually produce a narrow-complex tachycardia with no discernible P wave. The rate is usually between 160 and 190 beats per minute. In a less common form of atrioventricular nodal reentrant tachycardia, the circulating wavefront proceeds in an antegrade fashion down the fast pathway and in a retrograde fashion up the slow pathway. In this form, inverted P waves ( Figure 2 ) are clearly visible in lead II of the electrocardiogram (ECG).
It is important to note that atrioventricular nodal reentrant tachycardia can result in a wide-complex tachycardia if the patient has preexisting bundle branch block.
Accessory Pathways Causing PSVT
Accessory pathways (Wolff-Parkinson-White syndrome) and other bypass tracts can cause PSVT. In patients with Wolff-Parkinson-White syndrome, a shortened PR interval and a slurred upstrike to the QRS complex “delta wave” on the resting ECG indicate the presence of an accessory pathway ( Figure 3 ) .
It should be noted that the resting ECG may be normal in some patients with Wolff-Parkinson-White syndrome, because of the inability of the accessory pathway to conduct in the antegrade direction. The usual mechanism of PSVT in this setting is antegrade conduction down the normal pathways through the atrioventricular node and retrograde conduction through the accessory pathway.
The ECG in an atrial arrhythmia with an accessory pathway usually shows a narrow-complex tachycardia at rates of 160 to 240 beats per minute. Delta waves are absent because the normal pathways are used for ventricular activation. Inverted P waves may be seen in the inferior leads. In a much less common form of PSVT, antegrade conduction is down the bypass tract and results in a wide-complex tachycardia.
Increased Automaticity Causing PSVT
Increased automaticity usually occurs when the atrium is enlarged, as in patients with chronic lung disease, congestive heart failure, or electrolyte and acid-base disturbances. Usually, the stretched atria fire irregularly, producing multiple premature beats that emanate from different areas of the atria. Because the foci for the ectopic beats are in multiple sites, the P waves vary in morphology, giving rise to the term “multifocal atrial tachycardia.”
The diagnosis of multifocal atrial tachycardia depends on the identification of an irregular rhythm with three or more different P-wave morphologies. The rate is usually between 130 and 180 beats per minute. Treatment is directed at correcting the underlying cause. Antiarrhythmic drugs are usually not helpful.
In most patients, PSVT is benign and self-limited. However, some patients can have angina, hypotension, and intense anxiety. The first step in the management of PSVT is to determine whether the patient is hemodynamically stable. If PSVT is sustained and there is any indication of instability (i.e., angina, shortness of breath, decreased level of consciousness, hypotension, or congestive heart failure), electrical cardioversion should be performed urgently.
If the symptoms are restricted to discomfort (e.g., palpitations and anxiety), conservative measures should be applied. Conservative management of PSVT can include both nonpharmacologic and pharmacologic measures ( Table 3 ) . 16
Vagal maneuvers to increase parasympathetic tone and slow conduction through the atrioventricular node should be the first approach. Patients should be taught some of these maneuvers for use in future episodes. They should also be instructed to avoid inciting factors, such as caffeine, tobacco, alcohol, pseudoephedrine, and stress. Carotid sinus massage can be attempted, but its role hasbecome more limited because of the effectiveness of drug therapy and the risk of embolism from carotid pressure in some patients.
The goal of pharmacologic management is to slow or block atrioventricular nodal conduction. Agents used for this purpose include adenosine (Adenocard), calcium channel blockers (verapamil [Calan] or diltiazem), and beta blockers (e.g., esmolol [Brevibloc]).
Adenosine is an ultra–short-acting agent that is cleared quickly (half-life of 1 to 6 seconds). This agent is given intravenously in an initial dose of 6 mg, which is followed by one or two 12-mg boluses. Adenosine works by reducing conductance along the slow antegrade pathway. Side effects include flushing, dyspnea, and chest pain. Because of the short half-life of adenosine, these effects are usually very brief and do not ordinarily result in complications.
One advantage of adenosine is that it lacks the negative inotropic effects of calcium channel blockers. Adenosine can also decrease the sinus rate transiently and produce a “rebound” sinus tachycardia. Adenosine should not be used in patients with heart transplants, because such patients may be too sensitive to its effects. 17
Calcium channel blockers can also be used to disrupt a reentrant pathway. Verapamil can be given in a 5- to 10-mg bolus over 2 minutes, followed by 10 mg in 15 to 30 minutes if the initial dose does not convert the arrhythmia. 18 Verapamil and other calcium channel blockers should not be used in patients with an undiagnosed wide-complex tachycardia, because of the risk of fatal hypotension or ventricular fibrillation if the arrhythmia is actually ventricular tachycardia and not PSVT. 19
Intravenously administered diltiazem is also effective. 20 Initial treatment consists of a bolus of 0.25 mg per kg administered over two minutes. A repeat bolus of 0.35 mg per kg given over two minutes can be administered 15 minutes later.
Esmolol, a short-acting beta blocker, can be given in an intravenous bolus of 0.5 mg per kg over 1 minute or in an infusion at a rate of 0.5 mg per kg per minute after an initial loading dose of 0.5 mg per kg. An advantage of esmolol over other beta blockers is its short half-life (four to five minutes), compared with the much longer half-lives (three hours or more) of most other beta blockers. Because of a similar depressive effect on left ventricular contractility, esmolol should be used with caution if initial treatment with a calcium channel blocker is not successful.
Other antiarrhythmic drugs, including quinidine, procainamide, flecainide (Tambocor), and amiodarone, may be used in patients who do not respond to initial medications. However, selective radiofrequency ablation is rapidly becoming the treatment of choice in this situation.
Long-term control of recurrent PSVT caused by atrioventricular nodal reentry may be achieved with pharmacologic therapy or radiofrequency ablation. Patients who have infrequent, well-tolerated recurrences may manage these episodes with self-administered physiologic maneuvers.
Radiofrequency ablation is now used early in the management of patients with PSVT caused by an accessory pathway (Wolff-Parkinson-White syndrome), atrioventricular nodal reentrant tachycardia, or atrial tachycardia. 21 The success rate for radiofrequency ablation is 95 percent in patients with an accessory pathway or atrioventricular nodal reentrant tachycardia, and approximately 80 percent in patients with atrial tachycardia. 21
Other Atrial Arrhythmias
Sinus arrhythmia.
Sinus arrhythmia is usually a normal event in young persons and athletes. In fact, it occurs with such high frequency that it may considered a normal variant rather than a true arrhythmia.
There are two forms of sinus arrhythmia. In the “respiratory” form, the RR interval shortens during inspiration and slows during expiration. Breath-holding eliminates the variation. In the “nonrespiratory” form, the same phasic variation is seen in the RR interval but is not related to respirations. This form of sinus arrhythmia occurs in elderly patients, patients with digoxin overdose, and patients with increased intracranial pressure.
Sinus arrhythmia is usually asymptomatic. Sometimes, however, the long pauses can cause dizziness or syncope. Treatment is usually unnecessary.
WANDERING ATRIAL PACEMAKER
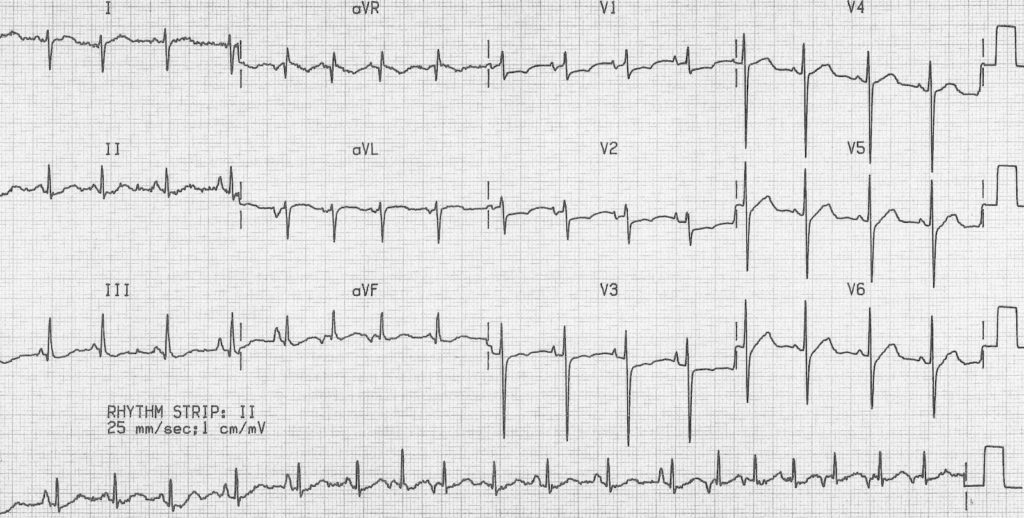
Patients with wandering atrial pacemaker are usually not symptomatic. The condition is most often an isolated finding on the ECG and requires no treatment. Sometimes it is noted on physical examination as an irregularly irregular rhythm.
With wandering atrial pacemaker, the ECG shows variable P-wave morphology and PR intervals. The atrial impulses conduct in a 1:1 fashion and usually control the rhythm for several beats before shifting to another focus. The normal heart rate in wandering atrial pacemaker differentiates this condition from multifocal atrial tachycardia.
PREMATURE ATRIAL COMPLEXES
A premature atrial complex is generated from an ectopic focus in the atria. Therefore, the P wave is usually different in morphology from the usual sinus P wave. The impulse conducts along the normal pathways, generating a narrow QRS complex followed by a pause. Sometimes the premature atrial complex is not conducted and can mimic heart block ( Figure 4 ) .
Premature atrial complexes are found in a variety of settings, including the excessive consumption of caffeine or alcohol and the use of sympathomimetic drugs. These complexes can also be present in patients with structural heart disease.
Patients with premature atrial complexes are usually asymptomatic and require no treatment. A beta blocker given in a low dosage can be tried in patients with uncomfortable symptoms, but no studies of efficacy have been reported. Patients should be counseled to decrease their intake of caffeine, tobacco, and alcohol, and their use of over-the-counter sympathomimetic substances, which are often present in cold medicines and weight-loss preparations.
It is important to note that premature atrial complexes sometimes precipitate supraventricular tachycardia, atrial flutter, or atrial fibrillation.
Sinus Nodal Arrhythmias
Sinus pause and sinoatrial exit block.
Sinus pause or arrest occurs when the sinoatrial node fails to discharge. The ECG shows a pause in the sinus rhythm, with no preceding P wave. Patients usually have no symptoms, but if the pause is prolonged, they may have lightheadedness, palpitations, syncope, and falls. In sinus arrest, the length of the pause has no relationship to the PP interval. Sinoatrial exit block is recognized by the pauses being multiples of PP intervals.
Sinus node dysfunction is usually caused by drugs such as digoxin, quinidine, or procainamide. It can also be caused by ischemia, myocarditis, or fibrosis.
From a therapeutic standpoint, it is probably not important to distinguish between sinus arrest and sino-atrial exit block. Both can occur in well-trained athletes 22 and can be a factor in sick sinus syndrome. 23
SICK SINUS SYNDROME
The term “sick sinus syndrome” encompasses a number of abnormalities, including sinus bradycardia, sinus arrest or exit block, combinations of sinoatrial and atrioventricular nodal conduction disturbances, and atrial tachyarrhythmias. More than one of these arrhythmias may be recorded in the same patient (bradycardia-tachycardia syndrome).
The abnormalities in sick sinus syndrome are usually due to ischemia, fibrosis, or drug-induced or autonomic dysfunction. Signs and symptoms are related to cerebral hypoperfusion and reduced cardiac output.
Treatment of recurrent symptomatic bradycardia or prolonged pauses requires implantation of a permanent pacemaker. 24
Levy S. Epidemiology and classification of atrial fibrillation. J Cardiovasc Electrophysiol. 1998;9(8 suppl):S78-82.
Ryder KM, Benjamin EJ. Epidemiology and significance of atrial fibrillation. Am J Cardiol. 1999;84(9A):R131-8.
Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840-4.
Golzari H, Cebul RD, Bahler RC. Atrial fibrillation: restoration and maintenance of sinus rhythm and indications for anticoagulation therapy. Ann Intern Med. 1996;125:311-23.
Pritchett EL. Management of atrial fibrillation. N Engl J Med. 1992;326:1264-71.
Sudlow M, Thomson R, Thwaites B, Rodgers H, Kenny RA. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet. 1998;352:1167-71.
Falk RH. Atrial fibrillation. N Engl J Med. 2001;344:1067-78.
Manning WJ, Silverman DI, Keighley CS, Oettgen P, Douglas PS. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J Am Coll Cardiol. 1995;25:1354-61.
Santos AL, Aleixo AM, Landieri J, Luis AS. Conversion of atrial fibrillation to sinus rhythm with amiodarone. Acta Med Port. 1979;1:15-23.
Management of new onset atrial fibrillation. Summary, evidence report/technology assessment: no. 12. Rockville, Md.: Agency for Healthcare Research and Quality, May 2000; AHRQ publication no. 00-E006. Retrieved April 23, 2002, from www.ahcpr.gov/clinic/epcsums/atrialsum.htm .
Falk RH, Knowlton AA, Bernard SA, Gotlieb NE, Battinelli NJ. Digoxin for converting recent-onset atrial fibrillation to sinus rhythm. A randomized, double-blinded trial. Ann Intern Med. 1987;106:503-6.
Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedo-mini G, et al. Circumferential radiofrequency ablation of pulmonary vein ostia: a new anatomic approach for curing atrial fibrillation. Circulation. 2000;102:2619-28.
Swerdlow CD, Schsls W, Dijkman B, Jung W, Sheth NV, Olson WH, et al. Detection of atrial fibrillation and flutter by a dual-chamber implantable cardioverter-defibrillator. For the Worldwide Jewel AF Investigators. Circulation. 2000;101:878-85.
Physicians' desk reference. 56th ed. Montvale, N.J.: Medical Economics, 2002.
Segal JB, McNamara RL, Miller MR, Kim N, Goodman SN, Powe NR, et al. The evidence regarding the drugs used for ventricular rate control. J Fam Pract. 2000;49:47-59.
Myerburg RJ, Kessler KM, Castellanos A. Recognition, clinical assessment, and management of arrhythmias and conduction disturbances. In: Alexander RW, Schlant RC, Fuster V, eds. Hurst's The heart, arteries and veins. 9th ed. New York: McGraw-Hill, Health Professions Division, 1998:873–942.
O'Nunain S, Jennison S, Bashir Y, Garratt C, McKenna W, Camm AJ. Effects of adenosine on atrial repolarization in the transplanted human heart. Am J Cardiol. 1993;71:248-51.
Rinkenberger RL, Prystowsky EN, Heger JJ, Troup PJ, Jackman WM, Zipes DP. Effects of intravenous and chronic oral verapamil administration in patients with supraventricular tachyarrhyth-mias. Circulation. 1980;62:996-1010.
Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986;104:766-71.
Betriu A, Chaitman BR, Bourassa MG, Brevers G, Scholl JM, Bruneau P, et al. Beneficial effect of intravenous diltiazem in the acute management of paroxysmal supraventricular tach-yarrhythmias. Circulation. 1983;67:88-94.
Morady F. Radio-frequency ablation as treatment for cardiac arrhythmias. N Engl J Med. 1999;340:534-44.
Bjornstad H, Storstein L, Meen HD, Hals O. Ambulatory electrocardiographic findings in top athletes, athletic students and control subjects. Cardiology. 1994;84:42-50.
Wu DL, Yeh SJ, Lin FC, Wang CC, Cherng WJ. Sinus automaticity and sinoatrial conduction in severe symptomatic sick sinus syndrome. J Am Coll Cardiol. 1992;19:355-64.
Haywood GA, Katritsis D, Ward J, Leigh-Jones M, Ward DE, Camm AJ. Atrial adaptive rate pacing in sick sinus syndrome: effects on exercise capacity and arrhythmias. Br Heart J. 1993;69:174-8.
Continue Reading
More in afp, more in pubmed.
Copyright © 2002 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.


- Mobile Apps
- Journal Club
- Antibiotics
- Quick Critical Care
- Residency Directory
- Recent Changes
- About WikEM
- Getting Started
- Creating & Editing
- Needed Pages
- Editorial Levels
- Contribution Score
- Elective Guide
- Citing WikEM
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Browse properties

- View source
- View history
- Create account

WikEM mobile app access is moving to Eolas! Our website will remain the same, but for mobile app users, this transition will offer an improved user interface, as well as additional in-app content such as MDCalc and a host of published guidelines. Download the free Eolas app now to ensure uninterrupted mobile app access.
- Wandering atrial pacemaker
- 2 Clinical Features
- 3.1 Palpitations
- 4.2 Diagnosis
- 5 Management
- 6 Disposition
- 8 External Links
- 9 References
- Three or more ectopic foci within the atrial myocardium serve as the pacemaker
- Rate is less than 100bpm (in contrast to MAT )
- Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia
- Intrinsic cardiac or pulmonary disease
- Metabolic derangements
- Drug toxicity (including Digoxin )
Clinical Features
- Often seen in the extremes of age and in athletes
- Rarely causes symptoms
Differential Diagnosis
Palpitations.
- Narrow-complex tachycardias
- Wide-complex tachycardias
- Second Degree AV Block Type I (Wenckeback)
- Second Degree AV Block Type II
- Third Degree AV Block
- Premature atrial contraction
- Premature junctional contraction
- Premature ventricular contraction
- Sick sinus syndrome
- Acute coronary syndrome
- Cardiomyopathy
- Congenital heart disease
- Congestive heart failure (CHF)
- Mitral valve prolapse
- Pacemaker complication
- Pericarditis
- Myocarditis
- Valvular disease
- Panic attack
- Somatic Symptom Disorder
- Drugs of abuse (e.g. cocaine )
- Medications (e.g. digoxin , theophylline )
- Thyroid storm
- Pulmonary embolism
- Dehydration
- Pheochromocytoma

- ECG should show three distinct P wave morphologies with a ventricular rate <100bpm
- Rarely requires treatment
Disposition
- Outpatient management
- Multifocal atrial tachycardia
- Dysrhythmia
External Links
- Richard Cunningham
- fardis tavangary
- Ross Donaldson
- Privacy policy
- Disclaimers
Wandering Atrial Pacemaker ECG Interpretation #312
Description.
- Rhythms are often named according to the origin of the electrical activity in the heart or the structure where the problem is occurring.
- Wandering Atrial Pacemaker is aptly named due to the electrical impulses causing the atrial activity are moving or wandering.
- These changes in the locus of stimulation affect the morphology of the P waves.
- In Wandering Atrial Pacemaker ECG, you must observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular.
- The PR interval is often affected, but does not have to be.
- The bottom line, is you must observe at least three different shaped P waves.
Practice Strip
Analyze this tracing using the five steps of rhythm analysis.
- Rhythm: Irregular
- P wave: Changing Shapes (3 or more)
- PR interval: Variable
- Interpretation: Wandering Atrial Pacemaker
Authors and Reviewers
- ECG heart rhythm modules: Thomas O'Brien.
- ECG monitor simulation developer: Steve Collmann
- 12 Lead Course: Dr. Michael Mazzini, MD .
- Spanish language ECG: Breena R. Taira, MD, MPH
- Medical review: Dr. Jonathan Keroes, MD
- Medical review: Dr. Pedro Azevedo, MD, Cardiology
- Last Update: 11/8/2021
- Electrocardiography for Healthcare Professionals, 6th Edition Kathryn Booth and Thomas O'Brien ISBN10: 1265013470, ISBN13: 9781265013479 McGraw Hill, 2023
- Rapid Interpretation of EKG's, Sixth Edition Dale Dublin Cover Publishing Company
- EKG Reference Guide EKG.Academy
- 12 Lead EKG for Nurses: Simple Steps to Interpret Rhythms, Arrhythmias, Blocks, Hypertrophy, Infarcts, & Cardiac Drugs Aaron Reed Create Space Independent Publishing
- Heart Sounds and Murmurs: A Practical Guide with Audio CD-ROM 3rd Edition Elsevier-Health Sciences Division Barbara A. Erickson, PhD, RN, CCRN
- The Virtual Cardiac Patient: A Multimedia Guide to Heart Sounds, Murmurs, EKG Jonathan Keroes, David Lieberman Publisher: Lippincott Williams & Wilkin) ISBN-10: 0781784425; ISBN-13: 978-0781784429
- Project Semilla, UCLA Emergency Medicine, EKG Training Breena R. Taira, MD, MPH
- ECG Reference Guide PracticalClinicalSkills.com

This website provides professional medical education. For medical care contact your doctor. 2024 ©MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us | 1

Thursday, March 4, 2021
Blog #200 — wandering pacemaker (vs mat).
There is no clinical information is available for the ECG and 2-lead rhythm strip shown below in Figure-1 .
- HOW would you interpret this tracing?
- What treatment is likely to be needed?
====================================
Editorial Comment:
It is always challenging to interpret tracings without the benefit of clinical information. That said — this situation is common in clinical practice. My experience in this area derives from the 30 years during which I was charged with interpreting all ECGs ordered by 35 medical providers at a primary care clinic — as well periodic stints during which I interpreted hospital tracings without the benefit of any history.
- The challenge lies with having to decide which tracings in the “pile of ECGs to be interpreted” were those for which I needed to pull the medical chart ( or call the provider ) because of ECG findings of immediate potential concern.
- Obvious time constraints made it impossible to pull the chart for each ECG that I was given to read ( I’d never get anything else done if I did so ).
- I therefore became well versed in the skill of limiting the charts that I would pull to those patients whose ECGs showed findings I thought were important and potentially indicative of an acute situation that may have been overlooked.
=====================================
MY Thoughts on the ECG in Figure-1:
As always — systematic interpretation of any ECG should begin with assessing the cardiac rhythm. In general — lead II and lead V1 are the 2 best leads on a 12-lead tracing for assessing atrial activity — and we have the advantage in Figure-1 of a simultaneously-recorded 2-lead rhythm strip of both of these leads. By the Ps , Qs and 3R Approach:
- The rhythm in Figure-1 is clearly irregular .
- The QRS complex is narrow ( ie, not more than half a large box in duration = ≤0.10 second ) .
- The rate varies from 50 /minute — to just under 100 /minute.
- More than 1 P wave morphology is present . That said — P waves do appear to be related to neighboring QRS complexes, because the PR interval for the P wave shapes that we see remains constant ( See Figure-2 ) .
MY Thoughts on Figure-2:
There are 2 different P wave shapes in Figure-2 .
- The tracing begins with 3 sinus beats ( ie, RED arrows highlight 3 similar-looking upright-in-lead-II P waves — all with the same PR interval ) .
- P wave shape then changes for beats #4, 5 and 6 ( ie, BLUE arrows highlighting an almost isoelectric, if not negative P wave with fixed PR interval ) .
- The atrial focus then shifts back , with return to sinus P waves for beats #7, 8, 9 and 10 (ie, return of RED arrows highlighting similar-looking, upright P waves in lead II — albeit with variability in the R-R interval ).
- The rhythm in Figure-2 concludes with a slowing-down of the ventricular rate, as the 2nd atrial focus returns , in which the P wave is almost isoelectric (ie, BLUE arrows for beats #11 and 12 ).
BOTTOM LINE regarding Figure-1: The rhythm in Figure-2 is most consistent with a Wandering Atrial Pacemaker . This is because the change from one atrial site to the next occurs gradually over a period of several beats.
- PEARL: The reason it is uncommon ( if not rare ) in clinical practice to see a wandering atrial pacemaker — is that most providers do not pay long enough attention to beat-to-beat change in P wave morphology needed to identify gradual shift between at least 3 different atrial sites.
SUMMARY: Review of the KEY features of wandering atrial pacemaker is the theme below for our ECG Media Pearl #17 ( a 3:30 minute audio recording ).
- Written review of wandering pacemaker appears below in Figure-3 .
- Review of MAT is covered in our ECG Blog #199 .

Today’s E CG M edia P EARL # 17 ( 3:30 minutes Audio ) — What is a Wandering Atrial Pacemaker ( as opposed to MAT )?
A DDENDUM ( 3/4/2021 ) :
I received the following note from David Richley regarding today’s tracing: “I think I would use different terminology to describe this because to me the atrial pacemaker doesn’t so much ‘wander’ as ‘jump’. I would describe this as sinus arrhythmia with junctional escape rhythm at 60-65/minute every time the sinus node discharge rate slows to below that rate. I interpret the escape beats as junctional rather than atrial, because athough the P waves, ( which are initially negative in II, aVF and V4-V6 — and positive in aVR ) precede the QRS — the PR segment is very short, suggesting an AV nodal origin. However, we describe this phenomenon — I do agree that it’s likely to be completely benign.
MY Thoughts: Dave’s comment is one of the reasons why: i ) The diagnosis of wandering pacemaker requires clear demonstration of shift in the atrial pacemaker in at least 3 different sites. We only see 2 different sites here; and , ii ) The diagnosis of wandering atrial pacemaker is not common.
- It’s impossible to rule out Dave’s theory from the single tracing we have.
- That said — the BLUE arrow P wave site may or may not be of AV nodal origin ( you can see a similar, near-isoelectric P wave with short PR interval from a low atrial site ).
- I also considered the possibility of the BLUE arrow P waves representing junctional escape — but decided against it because the difference in R-R interval from what we see between beats #9-10 vs what we see between beats #10-11 is more than what I’d expect based on the cadence of rate variation I see from beats #7-10.
- Bottom Line: We both agree there is a shift in the pacemaker site in a rhythm that is likely to be benign. And, we both agree that additional monitoring would be needed for a definitive response. THANK YOU Dave!
No comments:
Post a comment.

Wandering Atrial Pacemaker EKG Interpretation with Rhythm Strip
Ekg features, wandering atrial pacemaker ekg interpretation example.
This website is only for professional medical education. Contact your doctor for medical care. 2024 © MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Find in topic
RELATED TOPICS
INTRODUCTION
The sinoatrial (SA) node represents the integrated activity of pacemaker cells, sometimes called P cells, in a compact region at the junction of the high right atrium and the superior vena cava. Perinodal cells, sometimes called transitional or (T) cells, transmit the electrical impulse from the SA node to the right atrium. Each of these cell types has distinct expression profiles of ion channels and gap junctions.
Given the architecture of the SA node, SA nodal dysfunction typically results from either abnormalities in impulse generation by the P cells or abnormalities in conduction across the T cells. SA nodal dysfunction is more commonly an acquired condition, but in some patients it can be inherited, with gene mutations having been described in some forms of inherited SA nodal dysfunction [ 1 ]. Patients with SA nodal dysfunction may be asymptomatic or highly symptomatic as in cases of sinus node dysfunction (SND).
Sinoatrial nodal pauses, arrest, and exit block will be discussed here. Additional details regarding the anatomy and electrophysiology of the SA node, as well as a discussion of the SND, are presented separately. (See "Sinus node dysfunction: Epidemiology, etiology, and natural history" .)
Sinus pause, arrest, and exit block may arise from hyperkalemia; excessive vagal tone; ischemic, inflammatory, or infiltrative or fibrotic disease of the SA node; sleep apnea; certain drugs (eg, digitalis). The causes of SND are discussed in detail elsewhere. (See "Clinical manifestations of hyperkalemia in adults" and "Sinus node dysfunction: Epidemiology, etiology, and natural history", section on 'Etiology' and "Obstructive sleep apnea and cardiovascular disease in adults", section on 'Other arrhythmias' and "Cardiac arrhythmias due to digoxin toxicity", section on 'Sinus bradycardia, tachycardia, block, and arrest' .)
In patients receiving one or more agents that depress SA node and atrioventricular (AV) node function, a syndrome of bradycardia, renal failure, AV block, shock, and hyperkalemia (BRASH), has been described [ 2,3 ]. Patients with BRASH are generally taking therapeutic doses of SA and AV node blocking medications, and the level of hyperkalemia may be mild. However, the severity of bradycardia (caused by sinus arrest and/or AV block) is generally greater than expected for either the dose/level of SA and AV node blocker or the level of hyperkalemia.
Ectopic Supraventricular Arrhythmias
Various rhythms result from supraventricular foci (usually in the atria). Diagnosis is by electrocardiography. Many are asymptomatic and require no treatment.
(See also Overview of Arrhythmias .)
Ectopic supraventricular rhythms include
Atrial premature beats
Atrial tachycardia, multifocal atrial tachycardia, nonparoxysmal junctional tachycardia, wandering atrial pacemaker.
Atrial premature beats (APB), or premature atrial contractions (PAC), are common episodic impulses. They may occur in normal hearts with or without precipitating factors (eg, coffee, tea, alcohol, pseudoephedrine ) or may be a sign of a cardiopulmonary disorder. They are common in patients with chronic obstructive pulmonary disease (COPD). They occasionally cause palpitations.
Diagnosis is by electrocardiography (ECG—see figure Atrial premature beat ).
Atrial premature beat (APB)
Image courtesy of L. Brent Mitchell, MD.
APBs may be normally, aberrantly, or not conducted and are usually followed by a noncompensatory pause. Aberrantly conducted APBs (usually with right bundle branch block morphology) must be distinguished from premature beats of ventricular origin.
Atrial escape beats are ectopic atrial beats that emerge after long sinus pauses or sinus arrest. They may be single or multiple; escape beats from a single focus may produce a continuous rhythm (called ectopic atrial rhythm). Heart rate is typically slower, P wave morphology is typically different, and PR interval is slightly shorter than in sinus rhythm.
Atrial tachycardia is a regular rhythm caused by the consistent, rapid atrial activation from a single atrial focus. Heart rate is usually 150 to 200 beats/minute; however, with a very rapid atrial rate, nodal dysfunction, and/or digitalis toxicity, atrioventricular (AV) block may be present, and ventricular rate may be slower. Mechanisms include enhanced atrial automaticity and intra-atrial reentry.
Atrial tachycardia is the least common form (5%) of paroxysmal supraventricular tachycardia and usually occurs in patients with a structural heart disorder. Other causes include atrial irritation (eg, pericarditis
Symptoms are those of other tachycardias (eg, light-headedness, dizziness, palpitations, and rarely syncope).
Diagnosis is by electrocardiography (ECG); P waves, which differ in morphology from normal sinus P waves, precede QRS complexes but may be hidden within the preceding T wave (see figure True atrial tachycardia ).
True atrial tachycardia
Vagal maneuvers may be used to slow the heart rate, allowing visualization of P waves when they are hidden, but these maneuvers do not usually terminate the arrhythmia (demonstrating that the AV node is not an obligate part of the arrhythmia circuit).
Treatment involves managing causes and slowing ventricular response rate using a beta-blocker or calcium channel blocker. An episode may be terminated by direct current cardioversion . Pharmacologic approaches to termination and prevention of atrial tachycardia include antiarrhythmic drugs in class Ia, Ic, or III. If these noninvasive measures are ineffective, alternatives include overdrive pacing and ablation .
Multifocal atrial tachycardia (chaotic atrial tachycardia) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is > 100 beats/minute. On ECG, P-wave morphology differs from beat to beat, and there are ≥ 3 distinct P-wave morphologies. The presence of P waves distinguishes multifocal atrial tachycardia from atrial fibrillation . Except for the rate, features are the same as those of wandering atrial pacemaker. Symptoms, when they occur, are those of rapid tachycardia. Multifocal atrial tachycardia can be due to an underlying pulmonary disorder such as chronic obstructive pulmonary disease coronary artery disease , and electrolyte abnormalities such as hypokalemia . Treatment is directed at the underlying disorder.
Nonparoxysmal junctional tachycardia is caused by abnormal automaticity in the AV node or adjacent tissue, which typically follows open heart surgery, acute inferior myocardial infarction, myocarditis, or digitalis toxicity. Heart rate is 60 to 120 beats/minute; thus, symptoms are usually absent. ECG shows regular, normal-appearing QRS complexes without identifiable P waves or with retrograde P waves (inverted in the inferior leads) that occur shortly before ( < 0.1 second) or after the QRS complex. The rhythm is distinguished from paroxysmal supraventricular tachycardia by the lower heart rate and gradual onset and offset. Treatment is directed at causes.
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences


Multifocal Atrial Tachycardia (MAT)
- Ed Burns and Robert Buttner
- Jun 4, 2021
Multifocal Atrial Tachycardia (MAT) Overview
- A rapid, irregular atrial rhythm arising from multiple ectopic foci within the atria.
- Most commonly seen in patients with severe COPD or congestive heart failure.
- It is typically a transitional rhythm between frequent premature atrial complexes (PACs) and atrial flutter / fibrillation.
AKA “Chaotic atrial tachycardia”
Electrocardiographic Features
- Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm).
- Irregularly irregular rhythm with varying PP, PR and RR intervals.
- At least 3 distinct P-wave morphologies in the same lead.
- Isoelectric baseline between P-waves (i.e. no flutter waves).
- Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent PACs).
- Some P waves may be nonconducted; others may be aberrantly conducted to the ventricles.
There may be additional electrocardiographic features suggestive of COPD.
Clinical Relevance
- Usually occurs in seriously ill elderly patients with respiratory failure (e.g. exacerbation of COPD / CHF).
- Tends to resolve following treatment of the underlying disorder.
- The development of MAT during an acute illness is a poor prognostic sign, associated with a 60% in-hospital mortality and mean survival of just over a year. Death occurs due to the underlying illness; not the arrhythmia itself.
Arises due to a combination of factors that are present in hospitalised patients with acute-on-chronic respiratory failure:
- Right atrial dilatation (from cor pulmonale )
- Increased sympathetic drive
- Hypoxia and hypercarbia
- Beta-agonists
- Theophylline
- Electrolyte abnormalities: Hypokalaemia and hypomagnesaemia (e.g. secondary to diuretics / beta-agonists)
The net result is increased atrial automaticity.
ECG Examples

Multifocal atrial tachycardia:
- Rapid irregular rhythm > 100 bpm.
- At least 3 distinctive P-wave morphologies (arrows).
MAT with additional features of COPD :
- Rapid, irregular rhythm with multiple P-wave morphologies (best seen in the rhythm strip).
- Right axis deviation, dominant R wave in V1 and deep S wave in V6 suggest right ventricular hypertrophy due to cor pulmonale.
Related Topics
- The ECG in COPD
- Right atrial enlargement (P pulmonale)
- Right ventricular hypertrophy
Advanced Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course : Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop . Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog .
- Zimmerman FH. ECG Core Curriculum . 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations , 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine . 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care . 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG . 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Robert Buttner
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library . Twitter: @rob_buttner
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
ECG Educator Blog
ECG Education to help save more lives @ECGEducator, @JasonWinterECG
- Published Articles
- Facebook ECG Group
- ECG FB Group
- ECG Educator FB Page
- ECG & Cardiology FB Page
- Medical illustrations
- ECG Rhythm Strips
- www./paypalme/ECG1
- ECG Study PDF’s
Sunday 13 November 2016
Wandering atrial pacemaker (wap).

No comments:
Post a comment.
Akıl Kartları
Pacemaker ritimleri: normal pacemaker i̇şlevi.
- 23 Haziran 2014
Melis Efeoğlu
Pacemaker bileşenleri.
Pacemakerlar şunlardan oluşur:
1. Nabız jeneratörü
- Güç kaynağı
- Kontrol halkası
- Aktarıcı / alıcı
- Anahtar (mıknatıs ile aktive)
2. Elektrod(lar)
- Tek veya çoklu
- Unipolar veya bipolar
Pacemaker Sınıflaması
- Pacemakerlar pace modlarının niteliğine göre sınıflandırılmaktadırlar.
- Sınıflandırma Kuzey Amerika Pace ve Elektrofizyoloji Kurumu (NASPE) ve İngiliz Pacing ve Elektrofizyoloji grubu (BPEG) tarafından geliştirilen pacemaker koduna göre yapılır.
- Birkaç kitap hala 1987’deki bir önceki versiyonu kullanmasına rağmen, NASPE/BPEG jenerik (NBG) pacemaker kodu en son 2002 yılında revize edilmiştir.
- Kod beş harfe kadar seri şeklinde ifade edilmektedir.
NBG Pacemaker Kodu (2002)
Sıra I: Pacelenen Odacık (atriyum ya da ventikül)
- Hangi Odacıkların paceli olduğunu gösterir.
Sıra II: Algılanan Odacık(lar)
- Pacemakerın doğal kardiyak elektriksel aktiviteyi algıladığı lokasyonu gösterir.
Sıra III: Algıya Yanıt
- Pacemakerların algılanan doğal kardiyak aktiviteye yanıtını gösterir.
- T = algılanan aktivite pace aktivitesinin tetiklenmesi ile sonuçlanır.
- I = algılanan aktivite pace aktivitesinin inhibe edilmesi ile sonuçlanır.
Sıra IV: Hız düzenlemesi
- Fizyolojik gereksinimleri, ör. fiziksel aktivite, karşılamak üzere dizayn edilen hız ayarlanması kabiliyetini gösterir. Sensörler titreşim, solunum veya asit-baz durumunu içeren değişkenleri hesaplayıp bunlara yanıt verebilir.
Sıra V: Çoklu yerleşimli pace
- Bir anatomik bölge içerisinde çoklu stimülasyon uygulamasına olanak tanır, ör. atriyum içerisinde birden fazla pace bölgesi veya biatriyal pace.
NBG Pacemaker Kodu (1987)
Sıra I-III:
- 2002 kılavuzları ile aynı.
Sıra IV: Proglamlanabilirlik / hız düzenleme
- Pacemaker kurulumu veya hız ayarlanması kabiliyeti varlığı için programlama seçeneklerini gösterir.
- Anti-taşidisritmi fonksiyonu varlığını gösterir. Yerini NASPE/BPED Defibrilatör Kodu almıştır.
Yaygın Paceleme Modları
- Atriyal paceleme (Sıra I = A) ve algılama (Sıra II = A).
- Eğer doğal atriyal aktivite algılanırsa paceleme inhibe olur (Sıra III = I).
- Eğer tanımlanan süreden önce algılanan doğal aktivite yoksa atriyal paceleme başlatılır.
- Sağlam AV iletimi ile birlikte olan sinüs düğümü disfonksiyonunda kullanılır.
- Atriyal talep (demand) modu olarak da adlandırılır.
- Ventrikül paceleme (Sıra I = V) ve algılaması (Sıra II = V).
- AAI moduna benzer ancak atriyumlar yerine ventrikülleri içerir.
- Kronik atriyal bozukluğu ör. atriyal fibrilasyon veya flutter, olan hastalarda kullanılır.
- Hem atriyum hem de ventrikülleri paceleme ve algılama kapasitesine sahiptir.
- En yaygın pace modudur.
- Ayarlanan sürede doğal atriyal aktivite yoksa atriyal paceleme ortaya çıkar.
- Atriyal aktiviteyi takiben ayarlanan süre içerisinde doğal ventriküler aktivite yoksa ventriküler paceleme ortaya çıkar.
- Atriyal kanalın işlevi, ventriküler aktiviteyi veya retrograd P dalgalarını doğal atriyal aktivite olarak algılamasını önlemek için atriyal ve ventriküler aktiviteyi takiben sabit periodlar boyunca askıya alınır.
Mıknatıs modu
- Pacemakera mıknatıs tatbik etmek mıknatıs modunu başlatır.
- Bu mod pacemaker ayarlarına ve üreticiye göre değişkenlik gösterir.
- Genellikle asenkron bir paceleme modu başlatır – AOO, VOO veya DOO.
- Asenkron mod doğal ritim hızından bağımsız olarak sabit hızda paceli uyarı gönderir.
- Asenkron ventrikül pacinde pacemakerın indüklediği ventriküler taşikardi riski mevcuttur.
- Defibrilatör deaktivasyonu ile sonuçlanan implante edilebilir defibrilatöre (ICD) mıknatıs uygulanmasından farklı olduğuna dikkat ediniz.
Pacemaker Yerleştirilme Kriteri
2002 Amerikan Kardiyoloji Koleji, Amerikan Kalp Vakfı ve Kuzey Amerika Pace ve Elektrofizyoloji Derneği kardiyak pacemaker implantasyon kılavuzlarına buradan ulaşılabilir.
Paceli EKG – Elektrokardiyografik Özellikler
Paceli hastada EKG’nin görüntüsü kullanılan pace moduna, pace elektrodlarının yerleşimine, aygıt paceleme eşiği ve doğal elektriksel aktivite varlığına bağlıdır.
Paceli EKG’nin özellikleri:
Pace spikeları
- Kısa süreli vertikal dikenler (spike), genellikle 2 ms.
- Tüm derivasyonlarda görmek güç olabilir.
- Amplitüd pozisyona ve elektrod tipine bağlıdır.
- Bipolar elektrodlar unipolar elektrodlardan daha küçük pace dikeni (spike) ile sonuçlanır.
- Epikarda yerleştirilmiş elektrodlar endokardiyal olarak yerleştirilmiş elektrodlardan daha küçük pace dikeni (spike) ile sonuçlanır.
Atriyal paceleme
- Pace dikeni P dalgasından önce gelir.
- P dalgası morfolojisi elektrod yerleşimine bağlıdır fakat normal görünebilir.
Ventriküler paceleme
- Pace dikeni QRS kompleksinden önce gelir.
- Sağ ventrikül pace elektrodu yerleşimi sol dal bloğu na benzer QRS morfolojisi ile sonuçlanır.
- Sol epikardiyal pace elektrod yerleşimi sağ dal bloğu na benzer QRS morfolojisi ile sonuçlanır.
- ST segmentleri ve T dalgaları QRS kompleksi ile ters doğrultuda (diskordan) olmalıdır. QRS kompleksinin büyük bitiş bölgesi ST segmenti ve T dalgasının izoelektrik hatta göre zıt tarafında lokalizedir.
Çift Çember Pace
- Paceleme başlayan bölgelere bağlıdır.
- Atriyal pace, ventriküler pace veya ikisinin özelliklerini gösterebilir.
- Pace dikenleri sadece P dalgasının, sadece QRS kompleksinin veya her ikisinden birden önce gelebilir.
Pace komplekslerinin yokluğu, yeterli doğal iletimi yansıtabileceğinden, her zaman pacemaker bozukluğu anlamına gelmez.
EKG Özellikleri
Ekg örnekleri, çift çember paceleme.
A-V sıralı pace:
- Her bir QRS kompleksinden önce atriyal ve ventriküler pace dikenleri görünmektedir.
- %100 atriyal yakalama mevcuttur – her atriyal pace dikenini takiben küçük P dalgaları görülmektedir.
- %100 ventriküler yakalama mevcuttur – her ventriküler pace dikenini bir QRS kompleksi takip etmektedir.
- QRS kompleksleri sol dal bloğu morfolojisi ile birlikte geniştir, sağ ventrikülde ventriküler pace elektroduna işaret eder.
- A-V sıralı pace – atriyal ve ventriküler pace dikenleri %100 yakalama ile birlikte her QRS kompleksinden önce gelmektedir.
- A-V sıralı pacein bir diğer örneği.
Ventriküler Paceleme
Ventriküler paceli ritim:
- Ventriküler pace dikenleri her bir QRS kompleksinden önce gelir (sadece belki kompleks #2 hariç – bu kompleksteki QRS morfolojisi, bu vurunun da paceli olduğunu düşündürecek şekilde, EKG’nin geri kalanı ile aynıdır).
- Atriyal paceleme dikenleri görülmemektedir.
- Altta yatan doğal ritim muhtemelen kaba atriyal fibrilasyondur – V1’de görülebilen birkaç adet muhtemel P dalgası mevcut ancak aksi takdirde atriyal aktivite kaotiktir.
- Ventriküler pace dikenleri QRS komplekslerin çoğundan önce gelir.
- 6. ve 7. vurular farklı bir morfoloji ile birlikte, daha dardır – bunlar pacelenmemiş (“yakalama”) vuruları olup, muhtemelen supraventriküler kökenlidir.
- Vuru #6’nın üzerine gelen bir pace dikenşi mevcut ancak morfolojisini değiştirmemiş görünmektedir – füzyon kompleksine dair kanıt yok.
- Ventriküler pace dikenleri her bir QRS kompleksinden önce gelir, çoğu da sağ ventrikül pace elektrodu ile uyumlu sol dal bloğu morfolojisi sergiler.
- 5., 6. ve 11. kompleksler daha farklı bir morfolojide ve daha dardır – bunlar, ventrikül eş zamanlı olarak hem pace hem de supraventriküler (doğal) impulslar ile aktive olduğunda oluşan füzyon atımları dır. Pace dikeninin nasıl kısaldığını ve eş zamanlı doğal impuls ile QRS süresinin nasıl daraldığını görebilirsiniz.
- Pace dikeni ile birlikte hala biraz füzyon hali olmasına rağmen, 4. kompleks muhtemelen bir supraventriküler yakalama vurusu dur.
Atriyal Paceleme
Atiyal paceli hastaların paceli EKG’sinde bazal taramalarda görülmeyen sıklıkla birinci derece AV blok veya Wenckebach iletimi kanıtları mevcuttur. Bunun nedeni atriyal pace ihtiyacı olan hastalarda çeşitli derecelerde AV düğüm disfonksiyonunun (ör. yaş ilişkili AV düğüm dejenerasyonu / altta yatan kardiyak durum / ameliyat sonrası iskemi/ AV düğüm bloke eden ilaçlar) yaygın olarak mevcut olmasıdır. Bu hastalar AV düğümün kaldırabileceğinden daha yüksek hızda pacelendiklerinde, AV düğüm yorularak paceli EKG’de birinci derece AV blok veya Wenckebach fenomeni ile sonuçlanır. Bu anormallik klinik olarak anlamlı değildir, hastanın kardiyak outputunun tehlikeye atılmamasını sağlar.
1. Derece AV blok ile birikte atriyal paceli ritim:
- 90 vuru/dakikalık düzenli pace dikenleri mevcut.
- Her pace dikenini, %100 yakalamaya işaret eden bir P dalgası takip etmektedir.
- P dalgaları ventriküllere uzamış PR mesafesi ile iletilmektedir (280 ms).
Wenckebach iletimi ile birlikte atriyal paceli ritim:
- 90 vuru/dakika hızında düzenli atriyal pace dikenleri mevcut; her birini %100 atriyal yakalamaya işaret eden küçük bir P dalgası takip eder.
- Buna rağmen, her P dalgası QRS kompleksi ile sonuçlanmaz – PR aralığı gitgide uzar, AV iletim başarısızlığı ile sonuçlanır (“düşen QRS kompleksleri”).
- Mobitz I iletim ile birlikte 2. derece AV blok mevcuttur (Wenckebach fenomeni).
- Mobitz I, hastanın AV düğümünün kaldırabileceğinden daha hızlı pacelenmesine bağlıdır – kendi 50-60 vuru/dak hızında sadece 1. derece AV blok mevcuttu.
Pacemaker Muamması
Bu EKG’de neler olup bittiğini çözebilir misiniz?
Yanıt ve yorum
- Birçok atriyal ve ventriküler pace dikenleri ile birlikte düzensizce düzensiz bir ritim mevcuttur.
- QRS komplekslerinin çoğunluğu geniştir ve öncesinde ventriküler pace dikenleri bulunur.
- Sol dal bloğu morfolojisi sağ ventrikülde yerleşik ventriküler pace elektrodu ile uyumludur.
Atriyal ve ventriküler pace dikenleri arasındaki değişken ilişki en iyi II. derivasyon ritim çizgisi incelenerek anlaşılabilir (aşağıda):
- 1. vuru dar – bu atriyal pace dikeni tarafından tetiklenen bir doğal ventriküler kompleks olarak görülmektedir. Bu AV iletimin bir dereceye kadar sağlam olduğuna işaret etmektedir (3. Derece AV blok mevcut olamaz).
- 9. vuru ritim çizgisinin geri kalanından tamamen farklı bir morfoloji ve aksa sahip olup aynı zamanda geniştir – bu bir ventriküler ektopik vurudur.
- 3, 6, 8, 10 ve 12. vurulardan önce hem atriyal hem de ventriküler pace dikenleri gelmektedir – Ardışık A-V pace.
- 2, 4, 5, 7 ve 11. vurulardan önce sadece ventriküler pace dikenleri gelmektedir. Atriyal pace dikenlerinin yokluğu pacemakerın doğal supraventriküler impulslara yanıt verdiğini göstermektedir.
- Farkedilebilir P dalgasının yokluğu ve oldukça düzensiz ritime bakınca, altta yatan doğal ritmin atriyal fibrilasyon olması muhtemeldir.
Bu mükemmel EKG’yi bize sağladığı için Dr. Harry Peterson’a çok teşekkürler!
- DDD pace ile atriyal fibrilasyon ve ara sıra olan ventriküler ektopi.
Yazar Katkıları
Metin (temel içerik): John Larkin
Resimler&EKG yorumları: Ed Burns
Çeviri: Melis Efeoğlu
Sayfa Düzenleme: Haldun Akoğlu
Destekleyenler
Bu ve benzeri sayfalarda yer alan içerik Lifeinthefastlane.com Global FOAMed Portalının EKG Kütüphanesi ve A’dan Z’ye EKG Tanıları kısımlarından çevrilmiştir. Bu vesileyle Acil Tıp eğitiminin yeni çağı olarak nitelendirirebileceğimiz FOAM hareketine katkıları ve bu yoldaki şevkleri için Lifeinthefastlane.com eş-editörleri Dr. Chris Nickson ve Dr. Mike Cadogan’a teşekkürü bir borç biliriz.
This page is translated as is from the ECG Library and A to Z by Diagnosis series of Global FOAMed Portal Lifeinthefastlane.com into Turkish. We would like to thank Lifeinthefastlane.com Co-editors Dr. Chris Nickson and Dr. Mike Cadogan for their enthusiasm and contribution to the new era of Emergency Medicine Education. Viva la FOAM!
Referanslar
- Brady WJ, Truwit JD. Critical Decisions in Emergency & Acute Care Electrocardiography. Wiley Blackwell 2009.
- Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B, Reynolds DW et al. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group. Pacing Clin Electrophysiol. 2002 Feb;25(2):260-4. PMID: 11916002
- Bernstein AD, Camm AJ, Fletcher RD, Gold RD, Rickards AF, Smyth NP, Spielman SR, Sutton R. The NASPE/BPEG generic pacemaker code for antibradyarrhythmia and adaptive-rate pacing and antitachyarrhythmia devices. Pacing Clin Electrophysiol. 1987 Jul;10(4 Pt 1):794-9. PMID: 2441363
- Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B , Reynolds DW et al. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group. Pacing Clin Electrophysiol. 2002 Feb;25(2):260-4. PMID: 11916002
- Chan TC, Brady WJ, Harrigan RA, Ornato JP, Rosen P. ECG in Emergency Medicine and Acute Care. Elsevier Mosby 2005.
- Gregoratos G, Abrams J, Epstein AE, Freedman RA, Hayes DL, Hlatky MA, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines/North American Society for Pacing and Electrophysiology Committee to Update the 1998 Pacemaker Guidelines. ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines). Circulation. 2002 Oct 15;106(16):2145-61.PMID: 12379588 Full Text
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice (6th edition) , Saunders 2008.
- Wagner, GS. Marriott’s Practical Electrocardiography (11th edition), Lippincott Williams & Wilkins 2007.
- * EKG , LITFL EKG Kütüphanesi
- # ekg , pacemaker
Bu Yazının Podcasti
Acilcinin sesi.
harika, bir yoğun bakımcı olarak çok işime yaradı elinize sağlık
- Yanıtlamak için oturum açın
Bir Yorum Ekle Yanıtı iptal et
Yorum yapabilmek için oturum açmalısınız .
- Wandering atrial pacemaker
Term Hierarchy
- C R O G V Wandering atrial pacemaker
Professional guidelines
Recent clinical studies, clinical prediction guides.

IMAGES
VIDEO
COMMENTS
Wandering Atrial Pacemaker (WAP) ECG Review | Learn the Heart - Healio
This rhythm is benign. This rhythm and multifocal atrial tachycardia are similar except for heart rate. The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity. Usually, it is associated with underlying lung disease. In the elderly, it may be a manifestation ...
Paroxysmal supraventricular tachycardia (SVT) is a rapid cardiac rhythm involving atrial or atrioventricular node tissue. Learn about the common types, causes, symptoms, diagnosis, and treatment ...
A wandering atrial pacemaker is a rare arrhythmia that shifts the control of your heartbeat from the SA node to other parts of your atria. It can cause irregular heartbeats, but usually doesn't ...
WAP is an atrial arrhythmia with shifting pacemaker site and changing P wave morphology. Learn about its causes, symptoms, treatment, and examples from EKG strips.
Wandering atrial pacemaker is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. It is often benign and asymptomatic, and can be diagnosed by an ECG showing at least 3 different P-wave morphologies in a single lead.
In this column, the cardiac rhythms known as wandering atrial pacemaker (WAP) and multifocal ectopic atrial tachycardia are considered. Unlike other atrial arrhythmias, such as atrial fibrillation and atrial flutter, these heart rhythms are not caused by intrinsic pathological conduction problems and are usually eliminated by correcting noncardiac underlying conditions, such as respiratory ...
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury. Keywords: wandering atrial pacemaker, voltage, electrical injury, arrhythmia, ampere.
Wandering atrial pacemaker is a rare arrhythmia caused by three or more ectopic foci within the atrial myocardium. It is irregularly irregular and often seen in the extremes of age and in athletes.
Wandering atrial pacemaker is an irregular rhythm with P waves that vary in shape. It is similar to multifocal atrial tachycardia but the heart rate is under 100 bpm. Learn more about atrial rhythms and practice ECG tracings.
The mechanism of the wire's migration from the right atrial epicardium into the LV remains unclear. It was found in the left heart fortuitously affixed to a mitral chord - preventing further travel in the aorta. Migration of retained pacing wires to the left heart is very rare but possibly due to direct perforation.
Technically, for a rhythm to be classified as a wandering pacemaker — there should be gradual shift between at least 3 different atrial sites.Since we only see 2 different atrial sites (highlighted by RED and BLUE arrows) in Figure-2 — we would need a longer period of monitoring to prove this rhythm is a wandering pacemaker.That said — wandering pacemaker is the most logical explanation ...
Learn how to identify wandering atrial pacemaker, an arrhythmia with changing p-waves and variable PR interval, on an ECG. See a sample EKG rhythm strip and the qualifying criteria for this condition.
Learn how to distinguish between wandering atrial pacemaker (WAP) and multifocal atrial tachycardia (MAT) on ECG, based on P wave morphology and heart rate. WAP and MAT are benign rhythms that may be caused by various factors and may require treatment.
Learn about the causes, symptoms, diagnosis, and treatment of atrial fibrillation, flutter, tachycardia, and other arrhythmias that affect the heart's upper chambers. Find out how to prevent stroke, improve heart function, and control your heart rate with medications or procedures.
Learn about the causes, symptoms, and treatment of SA nodal dysfunction, which affects the pacemaker cells of the heart. This article covers sinus pause, arrest, and exit block, as well as the syndrome of bradycardia, renal failure, AV block, shock, and hyperkalemia (BRASH).
Summary Wherein the characteristic features of a wandering atrial pacemaker are identified Wandering Atrial Pacemaker - Field Guide to the Arrhythmias - Wiley Online Library Skip to Article Content
Wandering atrial pacemaker is one of the ectopic supraventricular rhythms that result from multiple ectopic atrial foci. It is an irregularly irregular rhythm with heart rate ≤ 100 beats/minute and no identifiable P waves on ECG.
A wandering atrial pacemaker is a specific arrhythmia that can affect the heart. A condition that affects the rhythm or rate of the heartbeat is known as an arrhythmia. There are wide varieties of arrhythmia, including an irregular beat, an extra beat, and a fast or slow heart rate.
MAT is a rapid, irregular atrial rhythm with multiple P-wave morphologies. It is often seen in COPD or CHF patients and has a poor prognosis. Wandering atrial pacemaker (WAP) is a similar arrhythmia with a single dominant pacemaker.
A wandering atrial pacemaker, (WAP), is an atrial arrhythmia that occurs when the natural cardiac pacemaker site shifts between the sinoatrial node (SA node), the atria, and/or the atrioventricular node (AV node).This shifting of the pacemaker from the SA node to adjacent tissues is identifiable on ECG Lead II by morphological changes in the P-wave; sinus beats have smooth upright P waves ...
Pacemaker Bileşenleri Pacemakerlar şunlardan oluşur: 1. Nabız jeneratörü Güç kaynağı Pil Kontrol halkası Aktarıcı / alıcı Anahtar (mıknatıs ile aktive) 2. Elektrod(lar) Tek veya çoklu Unipolar veya bipolar Pacemaker Sınıflaması Pacemakerlar pace modlarının niteliğine göre sınıflandırılmaktadırlar. Sınıflandırma Kuzey Amerika Pace ve Elektrofizyoloji Kurumu ...
Wandering atrial pacemaker (195101003) Definition. An electrocardiographic finding of a supraventricular arrhythmia characterized by 3 or more distinct P wave morphologies with an isoelectric baseline, variable PR intervals and no predominant atrial rhythm. The ventricular rate is typically below 100 beats per minute. (CDISC) [from NCI]