Our Locations


Cutting edge care for emotional trauma and mental health challenges.
Our protocols pair in-office medical treatments for mental health with virtual integration therapy to bring dramatic healing in the window of transformation following treatment.
Today only!
Try a month of our new Hybrid Program FREE . If you're suffering, let this be the beginning of your journey.

In-person Program
Accelerate your healing.
Our immersive in-person ketamine programs are the fastest track to help you reach deep breakthroughs and heal the root of your pain.
Hybrid Program
Start your path to lasting change.
Our holistic, hybrid journey blends ketamine, therapy, meditation, and wellness support in a flexible program that you can complete in-clinic or from the comfort of your home.
.jpg)
Stellate ganglion block
Dual Sympathetic Reset
Field Trip will soon be offering Stella's Dual Sympathetic Reset (DSR) protocol, an advanced Stellate Ganglion Block (SGB) treatment, at its NY and DC locations. This treatment has been shown to relieve symptoms of anxiety, depression, and PTSD/PTSI.

TRANSCRANIAL MAGNETIC STIMULATION (TMS)
FDA-approved treatment for depression.
Biological treatment for depression that’s rooted in brain science. Shown to provide relief for symptoms of major depression disorder through magnetic pulses that regulate activity in the prefrontal cortex.

Self-Guided Program
Explore your inner-self.
Our Field Trip app guides you in connecting with yourself and transcending consciousness, through music, meditations, and tools, created by leaders in mindfulness and psychedelics.

Stay Connected.
Sign up for our email newsletter where we share the latest news, education, events, and research in the psychedelic space.

by Luis Tamani
For Tripsitters, Therapists, and Guides: Tips & Resources
Practice supporting others on their journeys
Spiritually mature, heart-centered psychedelic guides are gems for humanity.
Here are some tips and resources for those seeking to grow in the work and serve as witnesses, mentors, and allies for other people's spiritual / psychedelic journeys.
Introduction
In recent years, many people have been called to be psychedelic therapists, guides, facilitators, or practitioners. This guide provides foundational advice and a curated list of resources to help us harness our full potential in such roles.
It's essential to approach this guide with a discerning mind. While the writer provides insights based on personal experiences and convictions, we invite each readyer to critically examine and question the perspectives presented.
One of the keys to thriving as a facilitator lies in communing with whatever medicine we serve. This commitment might mean going on journeys, fostering relationships with fellow guides, therapists, and tripsitters, and volunteering at or contributing to ceremonies and retreat centers that uphold high professionalism and ethics.
As with many pursuits, consistent practice strengthens our abilities. We naturally cultivates confidence and expertise by immersing ourself in both personal psychedelic experiences and supporting others in their journeys.
Embarking on our personal journey of discovery and initiation is foundational. Every experience and every step we take offers a more refined understanding and perspective. A mature facilitator knows that leadership comes from setting an example. Not cultivating a strong personal relationship with the medicine can hinder progress and diminish the abilities of our role as a guide.
Every interaction with the psychedelic realm can be seen as a revolutionary act, pushing against the confines of societal conditioning and reshaping our psyche. But this transformative journey demands introspection. How can we guide others through theirs if we shy away from confronting our personal shadows and fears?
The path of medicine work will inevitably highlight our weaknesses and the limits of our abilities. The question then becomes: Do we have the honesty and courage to see them? Or will we choose to overlook or deny them? Growth as a person and a facilitator stems from an unwavering commitment to self-awareness and authenticity.
There are three things you can do to help someone. The first is to listen. The second is to listen. The third is to listen some more.
The heart-centered path of the psychedelic guide.
Faith and commitment lay the foundation for anyone aspiring to delve deep into psychedelic medicine. Serving others and letting go of personal attachments unlocks opportunities, allowing us to fully immerse ourself in transformative work. Through the guidance of the medicine, we find our path illuminated. It refines our intentions, kindles the flame of gratitude, banishes lingering doubts, and ushers our awareness into the present moment.
It is paramount to nurture and fortify spiritual practices that foster qualities like compassion, generosity, loving-kindness, and experiential wisdom. A well-grounded practice equips us to be present and content without being trapped by endless desires or societal pressures to be something other than our authentic selves. This foundation empowers us to care for our well-being, establish boundaries, and self-reflect.
A heart filled with abundance and peace, content in its essence, can be fully present for others. When we're secure and joyous, we can open up, listen, and be present, creating a nurturing space for others. However, if our motivations sway towards chasing accolades, wealth, or validation, our efficacy as facilitators diminishes. By releasing such desires, we become a hollow-bone witness, not just for others but for our own journey.
Continuous growth requires vigilance against the mental toxins that might harm us and those we guide. As the Buddhist sage Shantideva puts it, "All the suffering in this world arises from wanting only ourselves to be happy. All the happiness in this world arises from wanting others to be happy." Genuine fulfillment and inspiration springs from a heart that gives generously, putting others' well-being at the forefront and serving as a beacon of love and understanding.
The journey down the medicine path is replete with challenges. In the early stages, confronting personal and shared traumas can seem daunting. The pain, confusion, and intense emotions might sometimes be overwhelming, tempting us to retreat. Yet, a deep, unwavering willingness to probe every nuance of our psyche is the hallmark of a dedicated practitioner. After all, if we shy away from facing our internal landscapes, how can we genuinely assist others in navigating theirs?
It’s best to get in the habit of being comfortable with cleaning up physical messes as a preliminary practice.
Navigating the depths: the calling of a psychedelic guide.
Understanding and alleviating the root of our suffering paves the way for love and light to shine through. As guides, the depth of personal introspection and healing we undertake directly correlates to the quality of the healing space we can offer others. By cultivating authenticity within ourselves, we foster a sanctuary where others can embrace vulnerability.
As one progresses on this journey, challenges may multiply. But a guide anchored in humility, compassion, and sincerity can navigate difficult terrain, drawing strength even from their missteps. Acknowledging errors, seeking forgiveness, and realigning with one's core purpose purifies the spirit.
While worldly allurements—chasing wealth, power, or recognition—might offer fleeting success, they often steer us away from genuine contentment.
Often, the most effective guides resonate with the teachings of the Tao Te Ching , exemplifying qualities like groundedness, humility, patience, and a deep-seated desire to serve. These practitioners understand the power of 'not knowing,' recognizing that true presence often means shedding intellectual confines to connect and feel more openly.
While writings from seasoned practitioners provide insights and reflections to budding guides, it's crucial to remember that literature serves only as a starting point. The practice of guiding is infinite and unpredictable; no amount of reading can wholly prepare one for its intricacies. Embracing each moment, continuously learning, and leading from the heart are the essential qualities of a dedicated and compassionate psychedelic guide.
Here are some texts that may be helpful:
Written Guides and Manuals
- Ground Control -- A Sitter’s Primer
- Zendo Psychedelic Harm Reduction Training Manual
- Psychedelic Crisis FAQ -- Erowid
- Psychedelic Trip Sitter Preparation Guide -- Tripsafe
- How To Tripsit in Real Life -- Tripsit.me
- How To Tripsit Online -- Tripsit.me
- How To Tripsit -- DoubleBlind
- The Psychedelic Trip Sitter’s Guide -- Zamnesia
- Manual of Psychedelic Support -- MAPS
- Developing Guidelines and Competencies for the Training of Psychedelic Therapists -- Janis Phelps
- Yale Manual of Psilocybin-Assisted Therapy of Depression
- MAPS Clinical Study Protocol
- Blossom: A Protocol for Psilocybin Assisted Self-Development
- Human Hallucinogen Research: Guidelines for Safety -- Johnson, Griffiths, Richards
- Handbook For The Therapeutic Use Of Lysergic Acid Diethylamide-25: Individual And Group Procedures
- Meeting the Divine Within: Using Psychedelic Wisely and Well -- James Fadiman
Codes of Ethics
It's essential to have a solid understanding of how a psychedelic therapist or guide is expected to think and act and some of the pitfalls to avoid.
- Council on Spiritual Practices
- American Psychological Association
- MAPS MDMA-Assisted Psychotherapy Code of Ethics
- The Conclave
- American Association for Marriage and Family Therapy
A true teacher will always point you back to yourself.
charting the path: training for the psychedelic guide .
Diverse training avenues exist for those drawn to the role of a psychedelic guide. It's important to navigate them with discernment, recognizing the richness and limitations of each.
Many established programs lean heavily on a Western medical and therapeutic model. This paradigm, like any, carries its biases. Historically, the Western approach has often been at odds with accepting psychedelic substances. Consequently, programs grounded in this mindset might impose restrictions such as preventing practitioners from directly experiencing the medicine or favoring academic qualifications over experiential wisdom— inadvertently perpetuating systemic biases.
Furthermore, such programs might emphasize individualism, sometimes overlooking the collective and holistic nature of healing. However, the insights gleaned from these Western-based modules can equip practitioners to thrive within contemporary society's framework, emphasizing the importance of being trauma-informed and understanding the nuances of the nervous system.
In stark contrast, indigenous cultures, some of which have embraced plant medicines for millennia, offer a more experiential path, albeit often without offering the formal certifications and diplomas recognized by Western institutions. Many modern practitioners have found immense value in immersing themselves with indigenous healers, absorbing ancient wisdom that challenges and enriches their foundational beliefs.
The medicine worker's path is versatile. Exposure to diverse cultural teachings often yields the most holistic approach. Supplemental practices like meditation, yoga, and breathwork could be equally, if not more, transformative than traditional clinical training. This path is a spiritual journey, transcending institutional norms and hierarchies.
Often, humble acts of service, like cooking or cleaning, become profound teachings. It primes one for the emotional and physical challenges of holding space. Indeed, in certain traditions, tasks like cleaning toilets are reserved for the highest masters, symbolizing humility and service.
Concluding with introspection: The essence of being a guide lies within you. Authentic mentors guide you inward, reinforcing your innate wisdom and abilities. Workshops, trainings, and retreats, in their truest sense, act as mirrors, reflecting your inherent potential and linking you to a community of like-minded beings.
“Holding space” means being physically, mentally, and emotionally present for someone.
As the third poem in the Tao says,
“If you overesteem great men,
People become powerless., if you overvalue possessions,, people begin to steal., the master leads, by emptying people's minds, and filling their cores,, by weakening their ambition, and toughening their resolve., he helps people lose everything, they know, everything they desire,, and creates confusion, in those who think that they know., practice not-doing,, and everything will fall into place.”.
- Alef Trust -- various training and degree and certificate programs in consciousness, transpersonal, and spiritual psychology
- Alien Insect -- youtube video series called Psychedelics and Brain Master Course
- Atma Academy Canada -- Accredited Psychedelic-assisted Psychotherapy Training Programs for Mental Health Professionals
- AWE -- hybrid three-year Psychedelic Therapy Training program offering MA and PhD tracks
- Aya Healing Retreats -- Various online and in-person training programs and apprenticeships, such as Trauma-Informed Plant Medicine Training Program and Somatic Plant Medicine Integration Training
- Being True to You -- Online Addiction Recovery and Psychedelic Integration Coaching Training
- Blossom Psychedelic Courses -- directory of courses and training programs
- California Institute of Integral Studies -- Hybrid Residential and Online Psychedelic-Assisted Therapies and Research Certificate Program (Boston or SF), 150 hours. Must have an advanced degree and licensure
- Canadian Psychedelic Association -- directory of courses and training programs
- Ceiba Ibogaine -- 4-part recorded series about Gabonese culture and the spiritual practice of Bwiti to educate and inspire anyone with an interest in the use of iboga
- Center for Optimal Living -- Live Online Integrative Harm Reduction Psychotherapy Certificate Program, and Intensive Trainings, CE credits available
- Center for Psychedelic Medicine (NYU) -- training programs in a clinical setting
- Chiron Academy -- Experiential, hands-on training in Canada
- Compass Pathways -- Online and clinical training for psilocybin therapy
- EntheoNurse -- various educational programs such as Psychedelics in Psychiatry
- Evolutionary Education -- live and online, trauma-informed training for helping professionals.
- Fluence -- various educational courses, workshops, and certificates such as Postgraduate Certificate in Psychedelic Integration Therapy.
- Gabor Mate -- various courses, events, and training programs with emphasis on compassionate inquiry and healing trauma and addiction
- The Guiding Presence -- pre-recorded online course with teachings from various practitioners
- Icahn School of Medicine at Mount Sinai -- lectures and clinical training for therapists
- Innate path -- 8-week Experiential, Cohort-based Psychedelic Training
- Institute of Psychedelic Therapy -- upcoming two-year psychedelic-assisted therapist training starting March 2022
- Integrative Psychiatry Institute -- Year-Long Online Psychedelic-Assisted Therapy Training with optional in-person ketamine experiential retreat
- IFS (Internal Family Systems) -- online courses and in-person trainings
- Inward Bound -- Online Introduction to Psychedelic Therapy Training Program
- Ketamine Training Center -- in-person workshop program is designed for experienced professionals
- MAPS Compilation of Institutions Offering Programs -- list of courses, programs, and institutions that offer education in psychology, psychedelics, transpersonal studies, etc.
- Maps MDMA Therapy Training -- virtual MDMA Therapy Training Program enrolls compassionate, experienced clinicians committed to health and well-being. Plans to host future in-person programs
- Microdose (Science of Psychedelics) -- accredited Professional Training in Psychedelic Medicine
- Mind Foundation -- various offerings such as in-person training in Germany and Amsterdam and recorded webinars and courses online
- Mind Medicine Australia -- Certificate In Psychedelic-assisted Therapies (CPAT), 90-hours hybrid program
- Naropa University -- The Naropa University Certificate in Psychedelic-Assisted Therapies is a ten-month, 200-hour non-degree training program featuring a hybrid delivery of online and retreat-based learning launching in 2022
- Nursing & Sacred Medicine -- online courses specifically for nurses of all levels of practice.
- Phoenix Academy -- psychedelic training programs in Vancouver
- Polaris Insight -- Ketamine and Psychedelic-Assisted Therapy Training
- Portland Psychotherapy Training -- Workshops and Classes for Therapists
- Psychedelic Coalition for Health -- in-person training in Los Angeles for healthcare professionals
- Psychedelic Insights -- experiential psilocybin retreat in the Netherlands for those who want experience sitting for others
- Psychedelic Medicine Association -- directory of courses and training programs
- PRATI (Psychedelic Research and Training Institute) -- In-person programs such as Ketamine and Psychedelic Medicine Training, for physicians and professionals
- Psychedelic Science at Berkeley -- Introduction to Psychedelic Science video series
- Psychedelics Sitter School -- several levels of online and in-person courses focused on therapeutic cannabis use but with broader applications to other psychedelics
- Psychedelic Somatic Institute -- Psychedelic Therapy Training and Apprenticeship
- Psychedelic Support -- Accredited courses to advance professional development and knowledge of psychedelic safety, therapeutic applications, and research findings
- Psychedelics Today -- Navigating Psychedelics for Clinicians and Therapists, 8-week Online Live Course
- Sage Institute -- two-year internship training program and a hybrid Ketamine-Assisted Psychotherapy Program
- Sarah Hope Coaching -- various courses, workshops, and retreats, such as Medicinekeeper Immersion, based in Colorado
- SCPTR (Salt City Psychedelic Therapy & Research) -- 8-week online Psychedelic Therapy Training Program
- Somastery -- trauma training for psychedelic facilitators
- Somatic Experiencing Trauma Institute -- training in the Somatic Experiencing modality
- Sophia University -- MA, PhD, PsyD, and certificate programs in various fields of Psychology
- SoundMind Center -- ten-week graduate-level training course for clinicians and other professionals
- Therapsil -- training program designed to train healthcare providers in how to safely and effectively guide a client on a therapeutic psilocybin experience
- University of Ottawa -- 9-credit Microprogram in Psychedelics and Spirituality Studies
- University of Wisconsin-Madison School of Pharmacy -- offering a masters-level program in Psychoactive Pharmaceutical Investigation and an online Capstone Certificate in Psychoactive Pharmaceutical Investigation
- Zendo Project -- variety of harm reduction resources
Here are some books that may be helpful on your path.
- The Ethics of Caring - Kylea Taylor
- The Art of Being a Healing Presence - Susan Cutshall, James E.Miller
- The Body Keeps The Score - Bessel van der Kolk
- Waking the Tiger: Healing Trauma - Peter A. Levine
- Grace Unfolding: Psychotherapy in the Spirit of Tao-Te Ching - Greg Johanson, Ron Kurts
Here are some videos that may provide insights into holding space for others.
- Zendo Project Psychedelic Harm Reduction - Volunteer Training 2014
- How to Work With Difficult Psychedelic Experiences - MAPS
- How To TripSit (Safety Guide) -- PsychedSubstances
- Dosed Documentary
- A New Understanding: The Science of Psilocybin
Articles :
Here are a few helpful articles about what we've discussed above.
- How To Become a Psychedelic Therapist
- Why More Therapists Need to Learn About Psychedelics—Now
If you think something should be added, changed, or taken off this guide, please email [email protected].
Explore written guides for journeyers .
Explore the mycelial network through the Tripsitters Directory .
To dive deeper, request a Consultation .
Let's stay connected
We’ll keep you in the loop.
Privacy Policy — Terms of Service
A bit about us:
Tripsitters belongs to humanity, the mushroom kingdom, and all of life. The mushroom partners with the tripsitters team to grow itself, spread healing, and gather community. The fungi are the visionaries, and our team follows their lead. We find joy in supporting the psychedelic revolution.
Keep in touch:

Made with ❤️ :
Design & Dev: Glenn and Alex Visionary Artwork: Luis Tamani
Design: Glenn van Roggen & Alex Dev: Alex Espinosa Visionary Artwork: Luis Tamani

Photo by Gravity Images/Getty
How to have a safe psychedelic trip
A psychedelic experience can be deeply rewarding, but also carries real risks. here’s how to avoid a bad trip.
by Christian Jarrett + BIO
is the editor of Psyche. A cognitive neuroscientist by training, his books include The Rough Guide to Psychology (2011), Great Myths of the Brain (2014) and Be Who You Want: Unlocking the Science of Personality Change (2021).
Edited by Sam Dresser
Listen to this Guide.
Need to know
Humans have consumed substances with consciousness-altering properties for millennia. Traditional societies used them in healing rituals, initiation ceremonies and to make contact with the gods and the dead, among other practices. Today they are known as psychedelics, and include the naturally occurring compounds psilocybin (found in ‘magic mushrooms’), DMT and mescaline; the hallucinogenic tea Ayahuasca, used by indigenous peoples in the Amazon basin; and the hallucinogenic shrub iboga, found in West Africa.
Synthetic hallucinogenic compounds, most famously LSD, emerged in the 20th century. The synthetic ‘party drugs’ MDMA (also known as ecstasy) and ketamine (used in medicine as an anaesthetic) are not technically classified as psychedelics, but they also produce consciousness-altering effects and are often considered under the same broad umbrella as the classic psychedelics.
In the industrialised West, psychedelic substances, especially LSD and magic mushrooms, burst on to the scene in the 1950s and ’60s with intense research interest in their therapeutic potential. However, an establishment backlash began in the late-1960s as the drugs became associated with the counterculture movement and opposition to the Vietnam War. Fermenting the eventual clampdown, the psychedelics-researcher-turned-evangelist Timothy Leary exhorted American youth to ‘turn on, tune in, drop out’. Tales spread of ‘bad trips’ and associated suicides, and the field of psychedelic research fell silent for decades.
We are now living through what’s been described as a ‘psychedelic renaissance’ that began in the 1990s. Research groups around the world, notably at Imperial College London and Johns Hopkins University in Baltimore, have been pumping out studies uncovering the neural basis of the drugs’ effects and exploring their apparent therapeutic benefits, especially when used as an adjunct to psychotherapy.
Research trials suggest that, when used as part of psychotherapy, the benefits of psychedelics include, but are not limited to, alleviating depression and anxiety (including for people who have not benefited from other forms of therapy or drug treatment), tackling longstanding symptoms of post-traumatic stress disorder, treating addiction, and calming existential distress in people with terminal illnesses.
Superior trial outcomes correlate with participants’ reports of having a mystical or transcendent experience during their psychedelic session. In fact, many people who take a psychedelic drug describe the experience as among the most personally meaningful of their lives. Many are changed by their trip, displaying greater open-mindedness, humility and feelings of connectedness with humanity and the wider world.
Although they can lead to subjectively similar experiences, different psychedelic drugs exert their effects in the brain via different mechanisms. For instance, psilocybin, mescaline and LSD act principally via the 5-HT2A receptor system (5-HT, also known as serotonin, is a neurotransmitter involved in mood and perception), whereas DMT acts on the 5-HT2A system and sigma-1 receptors involved in neuronal signalling. Meanwhile, ketamine interacts with another brain chemical called glutamate by blocking the NMDA receptors that this neurotransmitter usually binds with.
At a global level, psychedelic drugs have in common that they increase levels of entropy in the brain by allowing for communication between neural regions that don’t usually interact, and reducing the activity of a group of neural areas known collectively as the ‘default mode network’, which is involved in self-conscious thought. It’s believed that these neural changes lead to ‘ego dissolution’ and facilitate the mystical feelings of oneness and transcendence that are common to many trips.
The upsurge in research interest in psychedelic drugs and reports of their transcendent, life-changing effects have led to a steady flow of newspaper stories documenting their potential, and the publication of a spate of popular books about psychedelics. As curiosity about these drugs and their beneficial effects continues to grow, it raises the question of whether it’s possible for individuals to take these substances safely – and, if so, how?
Safety and legality issues
There are certain physical and mental health conditions that make it inadvisable to experiment with psychedelics, including heart problems and a history of psychosis or bipolar disorder. Antidepressant or antipsychotic medication could also interact unpredictably with the psychedelic. ‘Chronically, SSRIs [a form of antidepressant] may reduce the effect of psychedelics while other antidepressants may have other effects. But at this point there’s just not enough known about the effect of other psychoactive drugs on psychedelics,’ explains Sandeep Nayak, a psychiatrist at Johns Hopkins who has trained as a facilitator in psychedelic research studies.
‘If you have underlying mental health concerns or are experiencing depression, anxiety, or any medical issues, talk to a psychedelic-friendly therapist or doctor before taking substances,’ advises Sara Gael, director of harm reduction at the Multidisciplinary Association for Psychedelic Studies (MAPS) in the United States.
Even if you are fully fit and healthy, experts unanimously say that it’s a bad idea to take a psychedelic drug on your own, especially if it’s your first time. Ben Sessa is a psychiatrist, based in the United Kingdom, who has been researching the therapeutic effects of psychedelics for more than 15 years. He rejects the framing of the question in terms of whether it is possible to have a safe trip. ‘It’s like: “Is a knife safe or dangerous?”, it’s a ridiculous question. It’s about risk/benefit analysis.’ But he, like others, warns against journeying solo.
‘There are more risk factors [on your own] because there isn’t somebody there to manage your feelings or your behaviour,’ he says. ‘More importantly, you could be disorientated, and try to get in your car and drive away. Anything from the most benign behaviour – going online and buying 200 kg of avocados – to much more dangerous, there’s nobody who is not high who is able to temper your behaviour and make sure things are okay.’ Psychedelics have a profound effect on cognition, perception and coordination and you should take care to be in a physically safe, controlled environment. You should not plan to be driving, walking in traffic, be in high places or other dangerous environments which require you to be alert and coordinated.
Ideally you should identify an experienced and trusted guide or therapist to work with you before, during and after your psychedelic experience. Many cities in the US, Europe and elsewhere have psychedelics societies and these can be a good place to begin your search for a guide. At a minimum, make sure you are with a trusted and competent friend to keep you as safe as possible for the duration of the drug’s effects (consider, for instance, that the mind-altering effects of LSD can typically last up to 12 hours).
Another glaring practical issue is that, in most jurisdictions around the world, psychedelic drugs are illegal and if you are caught in possession, you will face criminal charges. This also has important implications for sourcing drugs safely. Françoise Bourzat, who has worked as a psychedelics guide in California for decades and is the author of the book Consciousness Medicine (2019), says that to source the drugs you will have little option other than to rely on word of mouth. ‘Always test your drugs,’ adds Gael. ‘Test kits are available on the DanceSafe website.’
If you decide to go ahead and it’s your first time, it’s sensible to start out with a weaker dose and, as mentioned, to pay due attention to the duration of the drug’s effects. The PsychonautWiki community encyclopaedia has information on dosing, duration and other practical issues.
However, even if you take these practical precautions, other experts urge an even more cautious stance. ‘I can’t and don’t endorse the use of psychedelics outside of research settings,’ says Nayak.
Fortunately, the physiological risks from the classic psychedelics are low to zero. ‘LSD and psilocybin are virtually inert physically – they have very low physical toxicity profiles so there are minimal physical risks,’ says Sessa. ‘They’re also not moreish,’ he explains. ‘You can see this in animal trials, they won’t repeatedly self-administer psychedelic drugs, they’ll take a single dose and then just largely ignore options to redose. So, the risk of addiction to psychedelics is low. Taking MDMA repeatedly long-term can be more harmful, but studies show that the physical risks go down after stopping.’
The main risks are psychological, and this is why preparation is so important. As safety guidelines for psychedelics trials from Johns Hopkins University put it: ‘The most likely risk associated with hallucinogen administration is commonly known as a “bad trip” and is characterised by anxiety, fear/panic, dysphoria, and/or paranoia.’
The most effective way to minimise the risk of a bad trip occurring is to prepare well. The Johns Hopkins advice is for guides and therapists to discuss the broad range of psychological effects that can be experienced under the influence of a psychedelic, including out-of-body sensations, the evocation of powerful memories, distortions to time and space, and feelings of oneness with the world, to name but a few. It’s also important to pay due attention to what Leary called ‘set and setting’. Most relevant to the preparation phase, ‘set’ describes the mindset and intention you bring to the psychedelic journey, and an experienced guide will work on this with you. The ‘setting’ refers to the physical, social and cultural environment in which the user takes a psychedelic drug.
‘Are you entering the experience with a certain need in your life? Do you want to explore something? Do you need healing? Do you have an emotional relationship that is problematic, burdened by childhood issues?’ asks Bourzat. ‘Do you want to be connected more with spirits or explore your relationship with nature? You don’t have to have a pathology to have an experience, but it’s a good idea to know why you’re doing it. What are you looking for in the journey? That’s the preparation.’ Other basic aspects of preparation, she adds, include writing a journal and preparing the body by fasting and avoiding alcohol.
The journey
Researchers have known about the importance of the ‘setting’ in the psychedelic experience for decades . In a series of studies published in 1960, Robert Hyde, a doctor at Boston Psychopathic Hospital, spent three years observing how the effects of LSD varied in different contexts. For instance, in the second year of his research, volunteers were treated as ‘research objects’ and given structured tasks to complete, whereas in the final year, the experience involved more chance for relaxation and personal support from and rapport with the researchers. Needless to say, the final year was generally associated with positive psychedelic experiences whereas the second year led to more unpleasant outcomes.
If you take a hallucinogenic drug at a party, even the attitude – the ‘set’ – of your friends could influence the ‘setting’ and thereby make a difference to your own experience. A field study in 2002 found that, on the rare occasions when people taking MDMA/ecstasy at parties reported bad experiences, this usually coincided with the user’s friends having pessimistic expectations or concerns about the trip. ‘A sense that another user, particularly a friend or acquaintance who is part of the collective, is not having a pleasant experience may have a deleterious effect on the group as a whole,’ the researchers said.
When it comes to a more formal, guided psychedelic journey, Bourzat explains that the setting is literally where the journey is happening: ‘What is the location? Who is sitting with you? Who is helping? What is the expertise and style of the guide? It also includes the length of time … What is guiding the work? Is it nature? Is it someone singing for you? Is there music playing? Is it quiet? All these different elements create the setting.’
She adds that commonsense steps to take include ensuring that the room is comfortable with soft furnishings and that any music is conducive to a pleasant experience. ‘I wouldn’t play rock and roll or house music. It should be expansive, not just classical but also more contemporary, or new age or tribal, African, Tibetan – anything ambient that’s conducive to introspection,’ says Bourzat.
If you have any frightening experiences or difficult overwhelming emotions, the usual advice is to surrender to these rather than trying to suppress them or run away from them. ‘Whether the disturbance consists of frightening illusions or internal imagery, difficult thoughts and feelings about some past or present personal issue, or anxiety related to a radical change in sense of self (eg, temporary loss of self-identity), the volunteer is encouraged to mentally surrender to the experience, trusting that her or his usual state of consciousness will return when the drug effects resolve,’ state the safety guidelines from Johns Hopkins University.
Integration
Following your psychedelic journey, it’s critical that you process the meaning of your experience with a guide or therapist. This ‘integration’ should take place during the two to three months after your experience. ‘When people take drugs recreationally, like just go to a festival and take LSD and then go home, that’s where they tend to run into problems because there’s a lack of integration of the experience,’ says Sessa.
One of the key aims of integration, Bourzat explains, is to carry the beneficial aspects of the psychedelic journey into everyday life. ‘If someone had a beautiful experience of nature, and in the journey they experienced beautiful birds, a meadow, then I would say you actually need to do that in your life. You need to cultivate that experience, and maintain that goodness that you connected with in the journey,’ she says. ‘Or say someone connected with a loved one they had lost, and felt love and tenderness and dealt with unfinished business in the journey, then I would suggest some ritual in real life – writing to the deceased person or beginning a journal and making that part of their life.’
Gael notes that integration therapists have different approaches and backgrounds. It’s important to find a guide or therapist whom you trust and who is nonjudgmental. ‘One helpful resource for finding integration support is the Psychedelic Support [network],’ she says.
Key points – How to have a safe psychedelic trip
- Remember that psychedelic substances are illegal in most jurisdictions.
- If you have physical or mental health issues, speak to a sympathetic doctor before experimenting with psychedelics. People with a history of psychosis or bipolar disorder are usually not allowed to participate in psychedelic research trials because they face heightened risks.
- Ensure you are in a physically safe, controlled environment. Always start with a low dose.
- Don’t take psychedelic drugs on your own. Find an experienced guide or therapist whom you trust.
- Use word of mouth at psychedelic societies and elsewhere to source psychedelic substances safely, and use online testing kits to ensure their quality. Alternatively, for greater safety, consider signing up to a research trial conducted at a university.
- Remember the importance of set and setting. Work with a guide who will help you prepare for your psychedelic journey, sit with you during the experience, and conduct integration with you for several weeks or months afterwards.
The main safety challenges confronting anyone who wishes to experiment with psychedelics stem from their illegality, meaning that there is no formal regulation of the training of psychedelic guides, nor is there a reliable way to source the drugs safely. Many researchers in the field, including Sessa, have been campaigning for drug-law reforms for decades. ‘The current situation is a total practical folly and extremely dangerous, utterly immoral and totally unpoliceable,’ he says. ‘It’s putting our heads in the sand and not addressing the fact that many people will take these drugs. It’s like the prohibition era in the States but on a much larger scale. The only way to control potentially dangerous drugs is through appropriate regulation. Imagine if scuba diving were outlawed – people would still do it, but now there were would be poor training, poor equipment and loads of people dying.’
Until the laws are changed, and outside of a research environment, the best route to a safe experience lies in finding a suitably trustworthy and experienced guide – someone who is vouched for by others. And it’s key that this guide will work with you before and after your psychedelic journey.
‘There’s lots of underground therapists in this country and elsewhere, these so-called healer/shaman/guru-type people who will quite happily take you down to Totnes and take four grand off you and take you into their yurt and give you a bag of mushrooms, but they won’t give you the other stuff; they won’t do the preparation and they won’t do the integration, so people are left hanging high and dry,’ says Sessa. ‘I always say to people who’ve found a so-called shaman or healer: “Ask this guy if he will see you for three weeks before and three weeks afterwards, and I bet he won’t.” That’s the bit that’s missing, not only from recreational use, but also from underground use.’
Until the laws change, signing up to a research trial is probably the least risky way to experience a psychedelic trip. These are being conducted at various research institutions around the world, principally: the University of Bristol, Imperial College London, Newcastle University and Manchester University in the UK; and at Johns Hopkins University in the US.
Links & books
Erowid is a US-based organisation that provides ‘reliable, nonjudgmental information about psychoactive plants, chemicals, and related issues’.
Bluelight is an ‘international, online, harm-reduction community committed to reducing the harms associated with drug use’.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is a US-based ‘non-profit research and educational organisation that develops medical, legal, and cultural contexts for people to benefit from the careful uses of psychedelics and marijuana’.
DanceSafe is a public health organisation, founded in California, that provides ‘a nonjudgmental perspective to help support people who use drugs in making informed decisions about their health and safety’.
PsychonautWiki is a ‘community-driven online encyclopaedia that aims to document the field of psychonautics in a comprehensive, scientifically grounded manner’.
The Psychedelic Renaissance (2nd ed, 2017) by Ben Sessa is an excellent introductory textbook that describes the cultural history of psychedelics, and is the most up-to-date review of contemporary work in the field.
Consciousness Medicine: Indigenous Wisdom, Entheogens, and Expanded States of Consciousness for Healing and Growth (2019) by Françoise Bourzat with Kristina Hunter is a ‘comprehensive guide to the safe and ethical application of expanded states of consciousness for therapists, healing practitioners, and sincere explorers’.
How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence (2018) by Michael Pollan is a ‘brilliant and brave investigation into the medical and scientific revolution taking place around psychedelic drugs – and the spellbinding story of his own life-changing psychedelic experiences’.

How to use ‘possibility thinking’
Have you hit an impasse in your personal or professional life? Answer these questions to open your mind to what’s possible
by Constance de Saint Laurent & Vlad Glăveanu
The nature of reality
How to think about time
This philosopher’s introduction to the nature of time could radically alter how you see your past and imagine your future
by Graeme A Forbes

How to control your gambling
What’s fun at first can all too easily get out of hand. Learn the warning signs and use these tips to rein things in
by Luke Clark
Premium Content
Psychedelic medicine is coming—but who’s going to guide your trip?
The U.S. may approve therapies using MDMA and psilocybin—aka ecstasy and magic mushrooms. The medical community is preparing for the deluge of demand.

Several years ago during a treatment for her lifelong depression with the psychedelic-like medication ketamine, Renee St.Clair was horrified to watch her brain disconnect from her body and float across the room.
“It was incredibly scary. I was really afraid it wasn’t going to come back,” the 51-year-old San Diego attorney recalls. The nurse attending her session quickly called in the psychiatrist, who verbally reassured St.Clair and squeezed her hand to make her feel safe. His soothing presence kept her calm during the 40 minutes until the hallucination passed and the drug was out of her system.
The importance of having well-trained professionals administer powerful psychedelic drugs is becoming urgent now. Not only will Oregon soon allow mental-health treatments with psilocybin—the active ingredient in magic mushrooms—but the United States Food and Drug Administration is expected to evaluate its first true psychedelic, methylenedioxy-methamphetamine (MDMA, aka ecstasy), for treating post-traumatic stress disorder later this year.
It was the realization that psychedelics might one day be integrated into mainstream medical care that spurred the California Institute of Integral Studies in San Francisco to become the first in the U.S. to offer a psychedelic-assisted therapy training program seven years ago, says Janis Phelps, director of the school’s Center for Psychedelic Therapies and Research.

In recent years, a growing number of institutions have followed. Psychotherapists, nurses, doctors, clergy, and others primarily in the mental health or spiritual professions are learning the chemistry of psychedelic molecules, safety concerns, historical Indigenous use, and, most importantly, the unique mental states unleashed by these drugs, whose effects last for six hours or more. But because psychedelics are currently illegal, no program enables participants to personally experience their effects.
Demand for these courses is booming, experts say, in large part due to a better understanding of the drugs’ potential mental health benefits. But national standards do not exist, leading to fears some graduates may have inadequate abilities as each institution create its own curriculum.
Inspired by promising clinical trials
Why are medical providers looking to MDMA as a potentially useful PTSD treatment? The powerful drug is thought to enable the brain to confront traumatic memories without triggering emotions like shame and rage, which can overwhelm and impede healing.
Preliminary results from the Multidisciplinary Association for Psychedelic Studies’ (MAPS) most recent large clinical trial confirm that two or three doses of MDMA reduced or eliminated PTSD. Most notable was that the effects persisted for six to 12 months. (These findings were released in April on MAPS’ website but have not been published in a medical journal.)
Positive results were also noted in MAPS’ first phase three clinical trial published in Nature Medicine in 2021, which showed that after three sessions of between 80 and 180 milligram doses of MDMA, three preparatory therapy sessions, and nine sessions post-medication, two-thirds of study participants no longer had PTSD.

Institutions around the world are revealing psychedelics’ promise for a range of mental-health disorders, including depression , anxiety , addiction , and reducing the fear of being diagnosed with a terminal disease.
Results like these inspired Anthony Back, a doctor at the University of Washington School of Medicine, to take the California Institute training in 2020. The 60-year-old Back says growing up in the 1980s around prominent antidrug ads kept him from experimenting in his youth. But the scientific research convinced him “there’s something really important here.”
In Back’s work as a palliative care physician, his primary goal is to reduce pain for patients with cancer. But “we haven’t had good ways of dealing with the terror” of learning your life is likely ending, he says.
How to administer a psychedelic drug
Institutions offering training programs vary greatly. Oregon has authorized nearly two dozen groups to conduct training for its statewide program, ranging from small facilities like the Earth Medicine Center to established universities including the University of California, Berkeley. Around the country, programs generally last six months to a year and cost thousands of dollars.
Most programs emphasize the importance of conducting multiple sessions before a drug is administered to discuss what patients hope to gain from the experience and what they might expect. Students also learn how to oversee the one or more sessions where the drug is administered. “The psychedelic experience is largely an internal one,” Phelps says, so therapists are taught not to interject themselves unless required to restore a sense of safety.
You May Also Like

9 simple ways to boost your mental health, according to science

8 strategies to make your New Year’s resolutions stick

What can your DNA say about your risk of opioid addiction?
Administering psychedelic-assisted therapy is vastly different for professionals used to conventional mental-health treatments, says Bit Yaden, a psychiatrist at Johns Hopkins Medicine, who is working on a pilot curriculum for Hopkins, Yale, and New York University psychiatry students. “When I prescribe Lexapro, my patient picks up the prescription and I hear in a month how it’s going,” she says. But with psychedelics, the actual dispensing of the medicine along with subsequent talk therapy are required, she says. During the many hours of a psychedelic session, one or more therapists must remain in the room.

Trainees are also taught how to help with a process known as integration, where patients incorporate insights and emotions from their psychedelic trip into their everyday lives. Here too, conventional therapists can find themselves in novel territory. “In psilocybin trials, there are reports of people having mystical experiences. Talking about those experiences may not have traditionally fit in a psychotherapeutic framework,” Yaden says.
Some programs have adopted the belief that therapists are best positioned to help others process powerful insights only after they have dealt with their own mental-health issues. That’s why Vancouver Island University in Canada offers a year-long training with numerous personal-development exercises and discussions to foster the personal and emotional growth of the therapist. “Using psychedelics is a way of remembering who you are,” says Geraldine Manson, a member of Canada’s Snuneymuxw First Nation who teaches in the program.
Training without psychedelics
Because psychedelics remain illegal, most programs are unable to have students facilitate an actual session with a psychedelic, an unfortunate limitation to their training, Phelps says. (Vancouver Island’s students, however, can do so because of government waivers allowing some mental-health patients to legally use the drugs.)
For the same reason, many students haven’t had personal experience with the drugs either. “It is clear when someone has never used a psychedelic. The types of questions they ask shows they have no idea what experience they’ll be providing to their patient,” says Pam Kryskow, medical chair of the Vancouver Island program.
Some encourage students to try ketamine under supervision to understand the extreme vulnerability of a being under the influence. Others attempt to simulate the state with a breathing practice known as Holotropic breathwork, which employs fast respiration to yield temporarily altered consciousness.
Some trainees seek out their own psychedelic experience with an underground guide or through by traveling to countries where Indigenous populations have long used the drugs. Palliative-care physician Back used a guide several years ago, an experience that prompted his desire to take the training. During the experience, as he later wrote in a medical journal, “my familiar sense of ‘me’—my preferences, my body, my history—dropped away, all at once, and what became palpable was an oceanic sensation of being unified with everything….There was a sense of being complete belonging…of having access to an energy in the universe that normally was hidden. It was exhilarating.”
Back believes such a framework would be helpful for his terminal patients. “I realized the process of dying was much more spiritual than I knew,” he now says, and he is eager for these drugs to be legalized.
Other medical professionals apparently feel similarly. In the California Institute’s first class of 42 students, several doctors and nurses insisted their participation be kept quiet to avoid potential harm to their professional reputations. But this year, some 800 people competed for the school’s 400 slots.
Despite the growth, experts worry there won’t be enough trained therapists to meet the expected demand after FDA approval of MDMA and possibly psilocybin, when thousands of professionals will be needed. In Oregon, not a single facilitator has so far met all criteria to be granted a license for psilocybin therapy.
"No training program is keeping up with the demand,” Phelps laments. Her university is developing a licensing program so other colleges can obtain the school’s training materials and videos, with some 25 already expressing interest, she says.
The only way psychedelics can succeed as a mental-health remedy is by ensuring enough professionals receive high-quality training, Back says. “This is a different kind of treatment than most others. Those are about the technology or the drug. Here, you have to have the therapy and the medicine together.”
Related Topics
- MENTAL HEALTH

We finally know the cause of severe morning sickness. A remedy could be next.

What’s behind extreme psychological reactions to eclipses?

Psychedelics may help treat PTSD—and the VA is intrigued

Being organized can actually improve mental health. This is why.

When will psychedelics be legal?
- Environment
- Perpetual Planet
- History & Culture
History & Culture
- History Magazine
- Mind, Body, Wonder
- Paid Content
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
To revisit this article, visit My Profile, then View saved stories .
- Backchannel
- Newsletters
- WIRED Insider
- WIRED Consulting
Margaret Rhodes
On Your Next Psychedelic Journey, Let an App Be Your Guide
“What type of Trip are you taking?”
The question appears on a phone screen, atop a soft-focus illustration of a dusky, Polynesian-seeming landscape. You could type in meditation or breathwork, or label it with a shorthand wink, like a mushroom emoji. The next question asks, “How far are you looking to go?” You choose “moderate”—you’re planning to ingest, say, 1.5 grams of magic mushrooms, which is still enough to make the bathroom floor tiles swirl like marbled paper. Select one of five prerecorded ambient soundtracks, and answer a few gentle questions about your state of mind. Soon you’ll be plumbing the depths of your consciousness, with an app as your guide.
It’s a capital-T Trip because the app belongs to Field Trip Health , a Toronto-based venture focusing on psychedelic-assisted psychotherapy. The Trip app , which begins a soft launch this week, is a digital companion to Field Trip’s clinics in New York, Los Angeles, and Toronto, where patients settle into rooms filled with Svago zero-gravity leather recliners and weighted blankets and take an ego-quieting psychedelic substance under the supervision of a Field Trip-trained therapist.
Field Trip belongs to a new and growing class of for-profit companies using psychedelic drugs (namely MDMA, ketamine, and psilocybin, the alkaloid that makes magic mushrooms magical) to treat depression, anxiety, and other obstinate mental illnesses. Unlike most players in that for-profit cohort, Field Trip is open for business. Field Trip isn’t dosing patients with MDMA or psilocybin; both are still listed by the government as Schedule 1 substances . But it’s also not waiting for legalization to find its customers. Instead, in New York and Toronto, Field Trip is treating select patients with ketamine, a dissociative drug that has FDA approval for off-label use right now. (The Los Angeles clinic opens later this month.)
And for those sheltering in place in the safety of the home, Field Trip's new app handily distills its consciousness-expanding protocols, making a guide—or at least a facsimile of one—accessible whether you can visit a clinic or not.
Psilocybin legalization is likely years away, but Field Trip cofounder Ronan Levy, a former executive at two Canadian cannabis companies, says the company plans to open 75 clinics in North America by 2024, if not sooner. “We’re building the infrastructure to support the coming wave, when psilocybin legalization efforts get across the line,” he says. “These experiences can be four, six, eight hours, and most doctor’s offices aren’t designed for that. You need a very different experience.”
For centuries, indigenous societies around the world have used psychedelic plants like psilocybin and ayahuasca in religious and societal ceremonies. The idea to study these substances and develop “best practices” for their use emerged in the United States in the late 1950s.
In 1957, a New York banker named R. Gordon Wasson wrote an article for Life magazine called " Seeking the Magic Mushroom ," based on several trips from deep in Oaxaca, Mexico. The article introduced untold Americans to the therapeutic possibility of psilocybin mushrooms, and a new avenue for self-improvement materialized. Psychedelics piqued the interest of researchers.
One such research initiative was Timothy Leary’s infamous Harvard Psilocybin Project, which administered doses of the drug to Boston-area graduate students between 1960 and 1962. Leary’s most lasting legacy (aside from coining the phrase “turn on, tune in, drop out,” and freaking the bejesus out of parents and politicians) is the concept of “set and setting.” Set refers to the mental state a person brings to the trip; setting refers to physical surroundings. Both require careful consideration for a trip to feel safe and insightful.
In many ways, Field Trip is packaging and franchising a kind of “set and setting.” This version includes carefully designed protocols (a consultation plus six ketamine-infusion sessions, combined with nine therapy sessions, for $4,700), digital touch points (an online portal where patients can prepare for their trips and chart their progress afterward), and ambiance (mid-century modern furniture, jute rugs, many, many potted plants). Soon, a Field Trip session might be like a Sweetgreen salad or a Heyday facial—it doesn’t matter which location you go to, because you’ll find the same menu of services and the same airy, placid ambiance wherever you end up. “You’ll never be walking into a room with tie-dye T-shirts and patchouli floating in the background,” Levy says. “We’re developing an experience that’s 100 percent controlled by us.”
Until recently, practitioners of psychedelic therapy clung to a loose set of aesthetics—hand-me-down tropes from the counterculture that grew slightly less cartoonish over time. In Michael Pollan’s 2018 book How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence , the therapeutic spaces he visits—at New York University and Johns Hopkins University, or in the homes of underground guides—almost invariably feature a Buddha figure or a ceramic mushroom in an otherwise unremarkable room.
These nostalgic, unpretentious environments make sense, given the landscape within which psychedelics have existed so far. Neither a clinical trial nor an underground (i.e., illegal) trip is much of a capitalistic venture. The marketplace is inherently limited: If you want to trip in the controlled company of a person, you either have to seek enrollment in a clinical trial or travel to a retreat in Mexico, Jamaica, or another country with different substance laws.
A theoretically more accessible option is an underground guide, but they’re hard to come by. “Even as someone who had their foot in the community, I had a hard time finding someone,” says Michelle Janikian, author of Your Psilocybin Mushroom Companion: An Informative, Easy-to-Use Guide to Understanding Magic Mushrooms . This is largely because psychedelic substances are illegal, but also because the resurgent attention to psychedelic therapy has led to a new crop of guides, many of whom lack training but still charge upwards of $1,000 for a session. Janikian describes meeting one such self-styled professional guide at a psychedelics conference. “When I got to know him he was just a normal person”—a guy in his forties, an ex-engineer—“who was changed by mushrooms and wanted to share them with others.”
Ketamine is only slightly more attainable. Patients with a doctor’s referral can visit one of many ketamine clinics across the United States, some more reputable than others. The Polaris Insight Center in San Francisco, for instance, was founded by clinicians from the Multidisciplinary Association for Psychedelic Studies (MAPS) and takes care to customize ketamine treatments for patients with varying dosages and talk therapy after a trip. On the flip side, a 2018 investigation by the science publication STAT found that many freestanding ketamine clinics fail to thoroughly screen patients, skip the integration step, and tend to oversell and overpromise, touting treatments like custom ketamine infusion “blends” based on a patient’s DNA.
Field Trip and its competition—companies like Compass Pathways , Mindbloom , and MindMed —present a new model for this kind of therapy, although actual access to these services varies. Compass has raised $116 million to run clinical trials for psilocybin treatment; MindMed is in the lab, developing medications based on psychedelic substances. Mindbloom, like Field Trip, offers in-clinic ketamine sessions as well as an at-home option; in that case, Mindbloom mails ketamine lozenges to its patients. (Field Trip will only administer ketamine in its clinics. If you use the Trip app to explore with drugs, you’ll have to procure your own substances.)

By Matt Simon
Ketamine has weathered a difficult reputation, first as a horse tranquilizer and then as a raver party drug, but it’s also widely used as an anesthetic and as an anti-inflammatory medication. It won’t occasion a colorful, hallucinogenic experience (like mushrooms do), but the right dose can put a person in a trance-like, dissociative state. “This facilitates the loosening of the habits in the mind,” says Joseph De Leo, Field Trip’s lead psychologist. “When an individual has a mystical experience, it provides them with a lot of material to process.”
Research on ketamine dates back decades. The Ketamine Papers , edited by Phil Wolfson (who has godfather status with the drug) and published by MAPS, documents those findings, many of which describe ketamine as an agent for spiritual processing. More recent studies from Yale and the National Institute of Mental Health home in on ketamine as a fast-acting treatment for depression. “For that, the science is good,” says Adam Kaplin, director of the Johns Hopkins Psychiatric Esketamine Clinic, before pointing out the problems: “We don’t yet know the best way to sustain the long-term benefits. It’s virgin territory. If patients don’t want to keep coming in and sitting in the clinic, what do we replace it with? We don’t know.”
Psychedelics can easily acquire an enticing sheen of before-and-after; even the very people developing long-range therapy programs will cite “an experience” that ended a depression or rewired a sense of self. The trick is what you do with the trip once it’s ended. In psychedelic-assisted therapy this is called integration, and it involves talk therapy, journaling, and goal-setting. “There’s actual work involved,” Levy says. “It’s not just, take this antidepressant and you’ll feel better .”
With Field Trip, much of that work takes place online, via a dashboard that tracks scheduled sessions, daily moods, goals, tasks, and perceived results. “It’s kind of like how One Medical has their own app,” says Kori Harrison, Field Trip’s head of product. A self-described “Silicon Valley type A person who saw the lights” after a few formative psychedelic experiences at Burning Man, she’s the bridge between Field Trip’s psychologists and its slate of tech products, including the Trip app.
Trip takes cues from journaling apps like Jour and Reflectly , and prompts users to take notes on their “narrative identity.” Harrison worked with Lucid—a company that uses machine-learning programming to compose music for “mental wellness”—on five custom, preprogrammed soundtracks. Each 45-minute track plays on a loop, mixing ambient music with nature sounds. Each selection is meant to facilitate a slightly different kind of emotional experience, from processing to healing to growth. (This is a theme among these new companies; Mindbloom also offers custom music.)
A red Record button sits front and center on the app's screen to let users take audio notes. Harrison heard from guides that patients find voice memos less overwhelming than journals. (“I wanted the app to feel like a beautiful oasis,” she says.) Trip technically doesn’t tout itself as a how-to guide for ingesting illegal substances—that would be against the rules of the App Store—but it mimics the work of a human guide, presenting calming visuals and encouraging introspection with multiple-choice questions like “How are you feeling right now?” Answers get saved in a journey log that can be accessed later.
Screens are a relatively new prop for psychedelic-assisted therapy. Experienced trippers caution against keeping a device around, for obvious reasons—just imagine picking up your phone to use Spotify, and instead winding up in a Twitter doomscroll while your drugs take hold—but digital interfaces could influence a trip in other, subliminal ways. In How to Change Your Mind , Pollan recounts a curious incident of looking at a computer during a guided mushroom trip. In an effort to try out some heady psycho-visual experiment, Pollan watches a video on his laptop mid-trip. Afterwards, eyeshades back on, he mentally finds himself in an “urban landscape that appeared to have been generated by a computer.” During his processing session the next day, Pollan’s guide suggests that the laptop screen inspired the computer-rendered hallucinations. “Could there be a better demonstration of the power of set and setting,” he asks.
If you follow that logic, then the media that’s consumed during a trip has a profound impact in shaping the visual tenor of what is typically an ineffable and unpredictable journey of the mind. Follow that logic further, and a more existential question emerges: With a specific animation and soundtrack in place, can you engineer a certain kind of trip? Would you want to?
For now, the Trip app makes a rarified toolkit much more accessible than before. While the app is useful for any kind of mood-tracking, Levy says it would be naive and insincere to pretend that people don’t self-medicate or explore at home—especially while many of us are stuck indoors, grappling with the ripple effects of a global pandemic. “This way, at least, we can make sure you have well-considered instructions,” Levy says. “I like to say we’re like Home Depot for self-exploration. You can do it, we can help.”
- How to outrun a dinosaur (just in case)
- Inside Citizen, the app that asks you to report on the crime next door
- The age of mass surveillance will not last forever
- A study finds sex differences in the brain. Does it matter ?
- These Black founders succeeded in spite of Silicon Valley
- 🎙️ Listen to Get WIRED , our new podcast about how the future is realized. Catch the latest episodes and subscribe to the 📩 newsletter to keep up with all our shows
- 💻 Upgrade your work game with our Gear team’s favorite laptops , keyboards , typing alternatives , and noise-canceling headphones
WIRED COUPONS

Extra 20% off sitewide - Dyson promo code

GoPro Promo Code: 15% off Cameras and Accessories

Get up to extra 45% Off - April Secret sale

10% Off Everything w/ Dell Promo Code

VistaPrint Promo Code: $10 Off $50+

50% off Select Products - Newegg Promo Code
- Conditionally
- Newsletter Signup
Health Conditions Chevron
Mental Health Chevron
- Panic Attacks
What’s the Safest Way to Try Psychedelic-Assisted Therapy Right Now?
By Nikesha Elise Williams

All products are independently selected by our editors. If you buy something, we may earn an affiliate commission.
Therapy and medication are currently the most powerful tools we have to treat mental health conditions like post-traumatic stress disorder (PTSD), depression, and anxiety, among so many others. But for some people—especially those who do not respond to these conventional treatments—researchers are discovering a promising new pathway to transformative mental health care: psychedelic therapy .
This isn’t the free-for-all glory days of Woodstock psychedelics that you might be imagining. We’re specifically talking about psychedelic- assisted therapy, which is practiced under the careful guidance of a trained clinician, who administers a controlled amount of a psychoactive substance to induce a person into an altered state of consciousness. In theory, this type of therapy encourages you to mentally explore the underlying roots of certain mental health issues. 1
It’s important to understand which drugs fall under the psychedelic umbrella: lysergic acid diethylamide (LSD, a synthetic chemical with hallucinogenic properties), 2 psilocybin (the psychoactive compound in magic mushrooms), 3 3,4-methylenedioxymethamphetamine (MDMA, often referred to as ecstasy or molly), 4 and ayahuasca (a mind-bending brew made from specific plants, which originated from Indigenous people in the Amazon Basin). 5 Because these are Schedule I drugs in the U.S., they are illegal at federal level due to their high potential for misuse and dependence, as well as having no accepted medical uses currently.
Then there’s ketamine, a Schedule III substance that is not typically seen as a genuine psychedelic. Instead it is viewed as a “dissociative anesthetic.” Currently, ketamine is the only substance with psychedelic properties with legalized, medically-accepted uses in the U.S. 6
Psilocybin is also on the path to legalization for therapeutic use, at least in Oregon , where it has already been decriminalized. Practically, that means the Oregon Health Authority will be responsible for licensing and regulating the manufacturing and sales of psilocybin products, as well as creating the country’s “ first regulatory framework for psilocybin services ” by January 2023.
The type of research experts have been able to do with these drugs has historically been limited—but significant strides are being made. In new and ongoing clinical trials, these substances have shown promise in treating everything from PTSD 7 to treatment-resistant depression 8 to substance use disorders. 9
Generally, in the future, once these drugs are approved by the U.S. Food and Drug Administration (FDA) for specific mental health conditions, psychedelic-assisted therapy might be considered when other largely effective treatments haven’t worked well for a person.
“We are entering a period where we can do expanded access treatment or compassionate use,” Monnica Williams, PhD , a clinical psychologist and training director of the Behavioral Wellness Clinic in Tolland, Connecticut, and a leader in the field of psychedelic science who has published over 100 peer-reviewed articles, tells SELF. “That’s when a drug is made available in advance of final approvals to people for whom nothing else has worked.” (We’ll dive more into this below.)
The experts SELF spoke with estimate it could take between 4 to 10 years for these drugs to receive FDA approval. But you shouldn’t let that timeline discourage you. Here’s everything you need to know about exploring this type of therapy right now.
What’s the safest way to access psychedelic-assisted therapy?
There are still a lot of hoops to jump through, but you have some options.
Ketamine is an injectable anesthetic that has traditionally been used for short-term sedation and anesthesia. But due to its dissociative and hallucinogenic effects, it’s been lumped in with other exploratory psychedelic research in the mental health space.
By Julia Sullivan

By Tatiana Walk-Morris

The FDA first approved esketamine , a ketamine-based nasal spray, for treatment-resistant depression in 2019. It is currently the only form of ketamine that is FDA-approved to treat a mental health condition and it is meant to be used in conjunction with antidepressants. Since esketamine can cause sedation, impaired judgment, and has the potential for misuse, there are strict guidelines around its use. It must be administered under the supervision of a doctor and you may need to convince your insurance to cover the cost by providing proof that you’ve tried other medications and therapies, according to Johns Hopkins Medicine .
Because ketamine is not a Schedule I drug, it is also prescribed for off-label use—say, to help treat other mental health conditions it was not specifically approved to treat, like PTSD. That loophole has given rise to ketamine-assisted therapy clinics all over the country, where ketamine is typically available via I.V. infusion.
You can walk into one of these clinics on your own, but you will need to do a mental health and medical evaluation to be approved for treatment. While these clinics are run by health professionals, concerns around safety and efficacy protocols—such as proper dosing—have been raised, as there is no regulated framework for ketamine-assisted therapy yet. 10 At these clinics patients are required to pay out of pocket since the use is considered off-label, and the price can range from hundreds to thousands of dollars, Peter Hendricks, PhD , a clinical psychologist and professor who specializes in substance abuse treatment and prevention and hallucinogenic therapy at the University of Alabama at Birmingham , tells SELF.
If you’re interested in ketamine, a good place to start is the American Society of Ketamine Physicians, Psychotherapists, and Practitioners (ASKP3) directory, as members of this organization pledge to uphold standards of practice and ethical principles when providing health care services.
One of the safest ways to try psychedelic-assisted therapy—whether you’re exploring MDMA, psilocybin, LSD, or other substances—is by participating in a clinical trial. That’s because the trials are done in a safe, controlled environment under the guidance of trained clinicians before, during, and after the psychedelic experience.
But being accepted into one of these clinical trials isn’t as easy as simply signing up. It’s a competitive space right now, Dr. Williams says. One clinical trial she’s leading, which is currently investigating MDMA for the treatment of PTSD, can only accept five people.
You also have to meet strict criteria to be considered as a trial participant, she says, which could involve having symptoms for a certain period of time, agreeing to all study rules and regulations, setting time commitments, and more. (While this looks different for each trial, here’s a snapshot of the qualifications you would need to meet to participate in trials spearheaded by the Multidisciplinary Association for Psychedelic Studies (MAPS) , a nonprofit research organization that investigates therapeutic uses for psychedelics and marijuana.)
To find a clinical trial near you, ask your doctor or therapist about any studies they might be aware of in your area. ClinicalTrials.gov is also a good resource; you can tailor your search to the type of psychedelic-assisted therapy and mental health issue you’re interested in, as well as your location. You can also look into accredited universities and medical centers that have research teams dedicated to psychedelics. Here are a few helpful places to start:
- Johns Hopkins Center for Psychedelic and Consciousness Research
- Massachusetts General Hospital Center for the Neuroscience of Psychedelics
- NYU Center for Psychedelic Medicine
- The Center for Psychedelic Psychotherapy and Trauma Research at Mount Sinai
- The University of Texas at Austin Center for Psychedelic Research and Therapy
- University of Wisconsin-Madison Transdisciplinary Center for Research in Psychoactive Substances
- U.C. Berkeley Center for the Science of Psychedelics
Expanded access means the FDA recognizes that a person has a serious or life-threatening condition that has not responded to other effective therapies, and the use of an “investigational medical product” could be appropriate to try if the potential benefits to the person’s quality of life outweigh the risks.
Unfortunately, it’s not a simple process. To get approval for expanded access treatment, you and your doctor will need to have a conversation about whether the treatment is a good choice for you, including the risks and costs to be aware of, according to the FDA . From there your doctor will need to seriously advocate for you by agreeing to oversee and monitor your treatment, reaching out to the company providing the medical product in order to receive its agreement, and submitting the necessary paperwork to the FDA. Once all parties agree to the expanded use request, treatment can begin.
For example, when it comes to expanded access to MDMA-assisted therapy to treat PTSD, at least two study sites are screening people for this purpose: Sage Integrative Health in California and the Pearl Psychedelic Institute in North Carolina. If your doctor believes this type of therapy may be the only way to treat your PTSD, they will need to contact an official expanded-access site on your behalf. Once the request and required medical information are received, the site will acknowledge the request within 10 business days and make a decision. Access is not guaranteed, even with a formal request, according to MAPS .
Let’s say you have already tried psychedelics on your own, in whatever capacity that may have looked like, and now you’ve got feelings about it. Thankfully, there are therapists who specifically work with people who have tried these drugs on their own and then felt like they needed to process the experience and the emotions it uncovered, Dr. Williams says. “We call it integration therapy,” she explains. “We do offer that because it happens a lot.”
The formal name for this type of therapy is psychedelic harm reduction and integration (PHRI). While many therapists work with people to process their psychedelic experience, there is no formal guidance on how to do this, according to a 2021 paper published in Frontiers in Psychology , which does provide a suggested framework. 11
According to the article’s authors, your therapist should help you process feelings that manifested during or after your experience, like anxiety, fear, or depression . Essentially, they should safely guide you through feelings of vulnerability, increased sensitivity, and other insights that arise. 11
When looking for an integration therapist, consider one who is trained in PHRI. Since it’s rooted in harm-reduction therapy—rather than abstinence-based approaches—PHRI-trained therapists won’t make moral judgments about drug use, so you should feel safe talking with them about your experience with psychedelics. 11 You may also want to ask about their knowledge of, or experience with, psychedelic-assisted therapy—as well as factors like their background and credentials, approach to treatment, and commitment to cultural competency —to determine if they may be a good fit for your personal needs and preferences.
Not sure where to begin? Inclusive Therapists has a directory that allows you to filter for experts who have experience in psychedelic-assisted or integration therapy in your area. Psychology Today and the American Psychological Association also have helpful directories for finding a therapist or psychiatrist in general.
As you may have noticed, we haven’t recommended obtaining or trying psychedelic drugs on your own to self-treat. Accessing them illegally and experimenting with them alone can be dangerous in various ways, Dr. Williams says.
There is a reason these substances are being explored carefully in the controlled setting of a clinical trial. Receiving the appropriate dose and working through your experience with a trained clinician is important for your physical and emotional safety and the effectiveness of the treatment itself. Outside of medically-approved settings, there’s no quality control for the substances being used and there’s no accountability for people who administer these drugs in a harmful way, Dr. Williams explains, even if any harm done is an accident. Unregulated practices can lead to a bad “trip” which has the potential to trigger or exacerbate mental or physical health issues—the opposite of what these drugs should be doing when used responsibly. In general, Dr. Williams says it’s just not worth it.
How are experts working to make psychedelic-assisted therapy more accessible in the future?
While researchers work to get these drugs closer to FDA approval, there’s been lots of buzz around future accessibility. Three big barriers include cost, therapy deserts, and a lack of diversity in researchers and trained professionals. Here’s where things stand now.
Like many novel treatments, psychedelic-assisted therapy is expensive. These sessions can run up to $20,000 to $40,000 or more, Dr. Williams, who has sought out grant funding to help lower the cost for her patients, says.
One way to lower cost, she says, is to tweak protocols without compromising efficacy, like reducing the number of required therapists in the room or the number of required sessions. Dr. Hendricks adds that telehealth psychotherapy sessions, subsidizing treatment for people who need financial assistance, or offering a sliding scale payment option could also help.
FDA approval could open the door to insurance coverage too. There are advocacy groups who are working to make sure that the necessary medical codes and billing procedures are ready, so these treatments can be billed to insurance when the time comes, Dr. Williams says.
Mental health care deserts continue to be a major problem in the U.S. 12 Add in the specialized training that will be required for psychedelic-assisted therapy, and the issue becomes even more challenging. When a framework for training is regulated and made accessible, it will be imperative to reach qualified practitioners and clinicians in all areas of the country.
There is also the question of how this training will be regulated. All eyes are on Oregon right now, Dr. Williams says, as the state’s health department has released draft guidelines for testing products and training requirements for people administering psilocybin. Currently, the draft guidelines state that facilitators will need a minimum of 120 hours of instruction, 25% of which needs to be in-person training, but the details are still being hammered out.
Dr. Williams says she once went to a research training and realized she was the only Black person in the room. “People were asking me, ‘How do we get more diverse participants in our studies?’” she recalls. For her the answer was simple: Diversify the study teams.
Diversifying the practitioners who are trained to administer these treatments is also imperative, she says. This means training people of all races, ethnicities, gender expressions, sexual orientations, and religious faiths.
If you’re from a marginalized community and have felt disrespected or dismissed by a health care provider in the past, then you understandably might have reservations about trying these therapies, “considering that you’re very vulnerable when you’re under the influence of psychedelics,” Dr. Williams says. “You’ll want to make sure you’re with somebody you can trust.”
- Frontiers in Pharmacology, Psychedelic-Assisted Psychotherapy: A Paradigm Shift in Psychiatric Research and Development
- StatPearls, Lysergic Acid Diethylamide (LSD)
- Molecules, The Therapeutic Potential of Psilocybin
- StatPearls, 3,4-Methylenedioxy-Methamphetamine Toxicity
- Currents of Neuropharmacology, Ayahuasca: Psychological and Physiologic Effects, Pharmacology and Potential Uses in Addiction and Mental Illness
- Department of Justice and Drug Enforcement Administration, Ketamine
- Nature, MDMA-Assisted Therapy For Severe PTSD: A Randomized, Double-Blind, Placebo-Controlled Phase 3 Study
- Journal of Psychopharmacology, Efficacy and Safety of Psilocybin-Assisted Treatment for Major Depressive Disorder: Prospective 12-Month Follow-Up
- International Journal of Drug Policy, Classic Psychedelics in the Treatment of Substance Use Disorder: Potential Synergies With Twelve-Step Programs
- Psychopharmacology Bulletin, Developing an IV Ketamine Clinic for Treatment-Resistant Depression: a Primer
- Frontiers in Psychology, Psychedelic Harm Reduction and Integration: A Transtheoretical Model for Clinical Practice
- National Rural Health Association, The Future of Rural Behavioral Health
- 13 Tips for Getting the Absolute Most Out of Therapy
- The Definition of Trauma Is Evolving—Here’s How That Can Help Us Heal
- 8 Things to Know Before You Try Ingestible Cannabis Products

SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is Psychedelic Therapy?
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Daniel B. Block, MD, is an award-winning, board-certified psychiatrist who operates a private practice in Pennsylvania.
:max_bytes(150000):strip_icc():format(webp)/block-8924ca72ff94426d940e8f7e639e3942.jpg)
Verywell / Alex Dos Diaz
Effectiveness
Things to consider, how to get started.
Psychedelic therapy is a technique that involves the use of psychedelic substances to aid the therapeutic process. Hallucinogenic substances have been used in holistic medicine and for spiritual practices by various cultures for thousands of years.
Research on the use of psychedelics flourished during the 1950s and 1960s until such substances were made illegal in the United States. While psychedelic drugs such as LSD and psilocybin are still illegal in the US, they are believed to have the potential to treat a range of conditions including anxiety, depression, and addiction.
Over the last two decades, researchers have gotten approval from authorities to conduct trials on the use of these substances to treat various conditions. For example, researchers have found that psilocybin is not only safe but that it can produce significant positive effects on well-being.
When utilized under supervision in a carefully controlled setting, research shows that some psychedelic substances can produce lasting and significant psychological and behavioral changes.
Types of Psychedelic Therapy
There are a number of different types of substances that can have psychedelic effects. Some common psychedelic substance and their uses include:
- Ayahuasca : This brew originating in South America is purported to help with addiction, anxiety, and depression. Possible side effects of Ayahuasca include serotonin syndrome and medication interactions.
- LSD : Lysergic acid diethylamide (LSD) can lead to altered mood, perception, and consciousness. Potential uses include the treatment of addiction and anxiety.
- Psilocybin : Like LSD, psilocybin alters consciousness, mood, and perceptions. It is being studied for its use in the treatment of addiction, anxiety, and depression.
- MDMA (ecstasy) : While not a classic psychedelic substance, MDMA (also known as ecstasy) is a drug that produces "psychedelic effects" including feelings of euphoria, altered perceptions, increased arousal, and increased sociability. Research suggests it has therapeutic potential in the treatment of post-traumatic stress disorder (PTSD).
Because there is no standardized method of administration and practice, individual practitioners have their own methods for administering psychedelic therapy. However, there are often a few common elements:
- Administration of a low to moderate dose of a psychedelic drug
- Supervision by a professional during the psychedelic experience
- Repeating the psychedelic dose with one to two weeks between sessions
During a psychedelic session, factors known as set and setting are critical. Set refers to things such as mood and expectations. Setting refers to the environment where the session takes place and the relationship with the therapist. The goal is to be comfortable with the therapist and the room where the session will take place. It is also important for patients to go into the experience feeling calm and attentive.
After the psychedelic experience, the focus at the next step is a process known as integration. These psychotherapy sessions are designed to help the individual process, make sense of, and find meaning in the psychedelic experience.
Microdosing
One variation of psychedelic therapy is known as microdosing , which involves taking very small, sub-hallucinogenic doses of psychedelic substances. Proponents of microdosing suggest that even these very low doses can have beneficial health effects such as enhancing performance, increasing energy, and decreasing depression.
While there is some evidence that microdosing may have some beneficial effects, more research is needed.
What Psychedelic Therapy Can Help With
Researchers have uncovered a number of potential applications for psychedelic therapy. Studies have found that anxiety, depression, substance use, alcohol use, and PTSD may all respond positively to psychedelic-assisted treatments.
- Anxiety and mood disorders : Psychedelics appear to have potential mood benefits that may be helpful in the treatment of depression. A 2016 randomized double-blind controlled trial found that psilocybin treatment led to significant reductions in anxiety and depression in patients undergoing cancer treatment.
- Alcohol and substance use disorders : Early research showed strong evidence that LSD could help in the recovery from substance use conditions. Some more recent evidence also supports the idea that psychedelic therapy holds promise as an addiction treatment.
- Post-traumatic stress disorder (PTSD) : Research also suggests that MDMA-assisted psychotherapy may be useful in the treatment of post-traumatic stress disorder (PTSD) . MDMA is best known as the main ingredient in the club drug ecstasy (or molly), but it also has psychedelic effects that have been shown to be useful for severe forms of PTSD that have not responded to other forms of treatment.
Press Play for Advice On Treating Emotional Pain
Hosted by Amy Morin, LCSW, this episode of The Verywell Mind Podcast , featuring psychologist Brian Pilecki, shares how psychedelics can be used to treat emotional pain. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts
Benefits of Psychedelic Therapy
Psychedelics are powerful substances that can produce profound mind-altering effects. These drugs are believed to work by affecting the neural circuits that use the neurotransmitter serotonin . Some of the potential benefits of these substances include:
- Feelings of relaxation
- Improved sense of well-being
- Increased social connectedness
- Introspection
- Spiritual experiences
It is important to remember that while psychedelics can produce positive benefits, it is also common for people to experience effects such as:
- Altered sense of time
- Distortions of reality
- Distorted perceptual experiences
- Intense perceptions or emotions
- Seeing, hearing, or sensing things that one would otherwise not experience
According to the National Institute on Drug Abuse (NIDA), these effects are a type of drug-induced psychosis that affects a person's ability to communicate with others, think rationally, and interpret reality. When used in a therapeutic setting where a trained professional can help a person understand and integrate these experiences, psychedelic therapy has the potential to help relieve the symptoms of certain psychiatric conditions.
After taking psychedelic substances, some people report having mystical or spiritual experiences. They may describe having feelings of peace, joy, unity, and empathy .
One study published in the Proceedings of the National Academy of Sciences suggests that the mood improvements induced by psychedelic drugs also appear to have lasting benefits. People who took psilocybin continued to experience improved well-being and increased social connectedness even after the substances wore off.
Psychedelic therapy shows a great deal of promise in the treatment of a wide variety of mental health conditions including addiction and depression. While further research is needed, current trials are underway to better determine the applications and effectiveness of using different psychedelic drugs to treat specific conditions.
Anxiety and Mood Disorders
Psilocybin-assisted therapy was also associated with increased quality of life, improved optimism, and reduced anxiety over mortality. About 80% of participants continued to show improvements six months later.
Another study looked at the effects of real-world psychedelic use by surveying music festival attendees. The participants reported that taking LSD and psilocybin helped improve mood and feel more socially connected. They also reported that these effects continued even after the drugs had worn off.
Alcohol and Substance Use Disorders
A 2015 study found that psilocybin-assisted therapy was associated with decreased drinking, reduced alcohol cravings , and increased abstinence. Psychedelic therapy's efficacy for alcohol and substance use has not yet been clearly established, however. One 2012 study found that a single dose of LSD had a beneficial effect on alcohol misuse up to six months after treatment, but the effects were not significant at the 12-month mark.
One 2019 study involved surveying people who had already quit using alcohol with the use of psychedelics. While only 10% of the respondents used psychedelics intentionally as a way to reduce alcohol use, more than 25% reported that the hallucinogenic experience played a role in changing their alcohol use.
It is important to note, however, that studies such as this are based on self-reports by people who have taken psychedelics in the past. In order to determine if psychedelic therapy is truly effective in the treatment of alcohol and substance use disorders , more research using randomized clinical trials is needed.
Post-Traumatic Stress Disorder
Clinical trials have demonstrated the treatment’s long-term efficacy in the treatment of PTSD. One study found that 54% of participants no longer met the criteria for diagnosis following treatment. Only 23% of participants in the control group no longer met the diagnostic criteria upon follow-up.
The benefits also appear to be long-lasting: 68% of those in the MDMA-assisted therapy treatment did not meet the diagnostic criteria for PTSD a year after treatment.
While psychedelic therapy is generally considered safe and is well-tolerated, there are some potential risks and adverse effects to consider. The classic psychedelics such as LSD and psilocybin pose few risks in terms of physical or psychological dependence along with other risks such as the following.
Negative Psychological Reactions
The potential for negative psychological reactions such as the symptoms of anxiety, panic, and paranoia is something to consider. The use of psychedelics can also result in what is known as a "bad trip." These experiences are marked by intense and terrifying feelings of anxiety and the fear of losing control.
Possible Personality Changes
Some have suggested that these drugs have the potential to produce long-term mind-altering, personality-changing effects. For example, one study found that psilocybin therapy was associated with increases in extroversion and openness . These findings suggest that people may become more outgoing and willing to try new things after being treated with psilocybin-assisted therapy.
Dangers of Self-Treatment
Another potential concern is the possibility of people using psychedelic substances to self-treat. Self-treatment can pose a number of risks including the psychological dangers of experiencing a bad trip, the possibility of drug interactions, and the fact that many street drugs are mixed with unknown and potentially harmful substances.
The effects that a person experiences with psychedelic substances can be unpredictable and can vary depending on the amount of the substance that is used as well as the individual’s personality, mood, and surroundings.
In 2019, the Food and Drug Administration (FDA) named psilocybin-assisted therapy as a "breakthrough therapy." This designation is designed to speed up the development and review of drugs that preliminary clinical trials have indicated treat serious conditions.
Currently, clinical trials into the use of LSD and psilocybin as treatments for alcohol dependence, anxiety, and depression are underway.
If you are interested in trying psychedelic therapy, signing up for a research trial is an option. You can search for clinical trials that are recruiting participants through the National Institute of Health (NIH) . The Multidisciplinary Association for Psychedelic Studies (MAPS) and the John Hopkins Center for Psychedelic and Consciousness Research may also sponsor research and trials that are accepting participants.
Never try to self-treat with psychedelics. In clinical settings, people are given a specified, pure dose, are supervised during the psychedelic experience, and receive professional help from a therapist to integrate the experience.
It is also important to note that while psychedelic therapy has demonstrated that it can be helpful in the treatment of a number of conditions, researchers are still exploring the exact mechanisms of action. Further research will allow scientists to figure out which drugs are most helpful for specific conditions, what doses should be used, and when such treatments should be avoided.
Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance . Psychopharmacology (Berl) . 2006 Aug;187(3):268-83;284-92. doi: 10.1007/s00213-006-0457-5
Mithoefer MC, Mithoefer AT, Feduccia AA, Jerome L, Wagner M, Wymer J, et al. 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for post-traumatic stress disorder in military veterans, firefighters, and police officers: A randomised, double-blind, dose-response, phase 2 clinical trial . Lancet Psychiatry . 2018;5(6):486–97.
Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial . J Psychopharmacol . 2016;30(12):1181-1197. doi:10.1177/0269881116675513
Denson R, Sydiaha D. A controlled study of LSD treatment in alcoholism and neurosis . Br J Psychiatry . 1970;116(533):443-5. doi:10.1192/bjp.116.533.443
National Institute on Drug Abuse. How do hallucinogens (LSD, psilocybin, peyote, DMT, and ayahuasca) affect the brain and body? .
Forstmann M, Yudkin DA, Prosser AMB, Heller SM, Crockett MJ. Transformative experience and social connectedness mediate the mood-enhancing effects of psychedelic use in naturalistic settings . Proc Natl Acad Sci USA . 2020;117(5):2338-2346. doi:10.1073/pnas.1918477117
Bogenschutz MP, Forcehimes AA, Pommy JA, Wilcox CE, Barbosa PC, Strassman RJ. Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study . J Psychopharmacol . 2015 Mar;29(3):289-99. doi:10.1177/0269881114565144
Krebs TS, Johansen PØ. Lysergic acid diethylamide (LSD) for alcoholism: Meta-analysis of randomized controlled trials . J Psychopharmacol (Oxford) . 2012;26(7):994-1002. doi:10.1177/0269881112439253
Garcia-Romeu A, Davis AK, Erowid F, Erowid E, Griffiths RR, Johnson MW. Cessation and reduction in alcohol consumption and misuse after psychedelic use . J Psychopharmacol . 2019;33(9):1088-1101. doi:10.1177/0269881119845793
Mithoefer MC, Feduccia AA, Jerome L, et al. MDMA-assisted psychotherapy for treatment of PTSD: Study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials . Psychopharmacology. 2019;236:2735–2745. doi:10.1007/s00213-019-05249-5
Erritzoe D, Roseman L, Nour MM, et al. Effects of psilocybin therapy on personality structure . Acta Psychiatr Scand . 2018;138(5):368-378. doi:10.1111/acps.12904
U.S. Food and Drug Administration. Breakthrough therapy .
American Cancer Society. Types and phases of clinical trials .
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."

Is the Trip Enough? Why Psychedelic Integration Therapy Is Important to Maximize the Benefits of Your Trip
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Share on Pinterest
- Share on LinkedIn
The main objective of integration therapy is to help individuals integrate the insights, emotions, and new perspectives gained from their psychedelic experiences, fostering lasting positive changes in their mental, emotional, and behavioral patterns.
In recent years, there has been a resurgence of interest in the therapeutic potential of psychedelic substances. Psychedelic integration therapy, a specialized form of psychotherapy, has emerged as a vital tool in the safe and effective use of these substances for personal growth, healing, and transformation. This article delves into the world of psychedelic integration therapy, exploring its principles, benefits, and the role it plays in maximizing the positive outcomes of psychedelic experiences.
Table of Contents
What is Psychedelic Integration Therapy?

Integration therapy is a vital, necessary part of any psychedelic trip that can help people reach their full potential. Source: Psych Central
Whether someone knows it or not, psychedelics offer a period after their trip that allows them to reexamine themselves and interpret the insights they got during their experience in the context of their lives. By examining these insights, individuals can begin to incorporate them into their daily lives, thus integrating them. This process of post-psychedelic trip introspection is called integration.
Psychedelic integration therapy is a therapeutic approach designed to support individuals in making sense of their psychedelic experiences and integrating them into their everyday lives. These experiences, induced by substances like psilocybin , LSD , or MDMA , often lead to profound shifts in perception, emotions, and consciousness. However, without proper guidance and processing, these shifts can be challenging to comprehend and integrate into one’s life. Psychedelic integration therapy is an active introspective process.
Key Principles of Psychedelic Integration Therapy
- Non-judgmental Space: Integration therapy provides a safe and non-judgmental space for individuals to share their psychedelic experiences openly. This allows them to explore and discuss any challenging or enlightening aspects of their journey without fear of criticism.
- Therapeutic Alliance: A strong therapeutic alliance between the therapist and the individual is crucial for effective integration. Trust and rapport allow for a deeper exploration of emotions and thoughts, enabling a more profound integration process.
- Personalized Approach: Each individual’s psychedelic experience is unique, and therefore, the integration therapy process is tailored to the specific needs, goals, and personality of the individual.
- Mindfulness and Self-Reflection: Integration therapy often incorporates mindfulness techniques and encourages self-reflection. These practices help individuals observe their thoughts and emotions without attachment and cultivate a deeper understanding of themselves.
- Creative Expression : Art, music, and other creative forms of expression are frequently employed in integration therapy. They can serve as powerful tools for individuals to externalize and explore the complexities of their experiences.
What Does Psychedelic Integration Look Like?
Psychedelic integration can look differently for everyone, depending on their individual experiences, goals, and environments. Source: Verywell Mind
Let’s say someone kept having important revelations and insight during their psychedelic experience around tapping into their creative energy. The related integration work surrounding this would be making a conscious effort in carrying that out, such as maybe starting a sketchbook practice, learning how to paint, or perhaps signing up for art classes. Anything that pushes someone to accomplish the insights a psychedelic experience showed them is part of psychedelic integration.
But psychedelic integration may not look the same for everyone. Everyone has radically different psychedelic experiences, so their integration will also reflect that. Some people may focus on more broader themes, such as making changes in their careers, relationships, or personality, whilst others may focus on smaller tasks, such as calling their parents to tell them they love them, or perhaps simply starting a new routine. For others, integration could be less concrete, such as someone deciding that want to start living authentically.
Regardless of how someone tackles integration, any method is valid and encouraged. The method one chooses depends on their own circumstances, their intentions for their trip, who they are as a person, and where they want to go in life.
Psychedelic integration therapy also looks differently depending on the therapist’s approach. A therapist’s professional training, culture, and identity will inevitably impact their approach to psychedelic integration, so integration therapy will never look quite the same across professionals.
Types of Psychedelic Integration
As mentioned, professionals have different ways of tackling psychedelic integration. Knowing the different types of methods that psychedelic integration can look like can help someone be better informed about what they want out of their therapy session.
Emotional Integration
Emotional integration is the practice of acknowledging and exploring the emotions and feelings that come up during a psychedelic experience and in a person’s life. A professional can help open someone up emotionally to let any pent up emotions they have kept inside them be released and processed. For example, someone may be harboring feelings of grief and need help releasing it from their psyche. Same thing may happen if they have been repressing forgiveness for someone else and need help in finally closing old wounds and moving past them.
Psychedelic experiences will inevitably provide insights into one’s emotional state and help certain repressed emotions rise to the top. A professional can help someone carry this emotional work out.
Somatic Integration
Conversely to emotional integration, a person may actually need a more physical integration process. This could be relating to insights regarding to health or ways to relieve stress. To aid in processing and integrating these insights, somatic integration highly focuses on the body and the sensations and feelings that arise. Some examples of this could be going for a walk, doing yoga or other forms of exercise, creating a workout routine and implementing it, and working on taking care of one’s physical or mental health.
Psycho-spiritual integration
Lastly, some insights may not be emotional or physical, but rather focus more on a combination of introspection and extrospection. A psychedelic experience may affect the way a person sees themselves, those around them, their surroundings, society, and reevaluate the relationship between themselves and all these things. There are various themes that can arise during a psychedelic trip that can cause someone to want to focus more on this aspect of their lives. Similarly, a psychedelic trip could also spur up feelings of existentialism and spirituality that may need to be integrated. Perhaps a person is confronted with their own feelings of death, of someone’s else’s impending death, or perhaps their relationship with religion and spirituality. All of these more introspective topics get addressed through psycho-spiritual integration by looking inward.
This type of integration may have a person asking what kind of person they are and what kind of person they want to be, question their relationships, question their purpose in life, and begin to push them to sift through what serves them and what doesn’t. This will ultimately lead to someone coming into a more authentic sense of themselves. Integration therapy helps people begin to reflect on these questions and answer them in order for them to them take decisive action and make questions into a reality.
How Long Does Psychedelic Integration Take?

Psychedelic integration therapy is a vital part of any trip and should not be rushed. Integration takes anywhere from a few minutes to a few years; it is not a race. Source: WebMD
This is a hard to question answer, as it depends on each individual, their intention, goals, and circumstances. Some integration activities could be handled rather quickly, such as calling a family member to express their love, changing a diet or creating a workout regimen, or signing up for classes.
Other integration activities take much longer, particularly those dealing with introspection and deeper themes that require more profound work with a therapist. There may not be a finish line for themes like these and integration looks more like an ongoing, lifelong process because a person constantly changes and their world is too, so the way they react to things will inevitably begin to shift.
Dealing with deeper emotional concepts like grief can be lifelong, for example; sometimes the grief may dissipate, and sometimes it may spur up and come and go like waves – integration in this context can be lifelong in order to acknowledge the feelings that bubble up and learn how to process them in whatever new context a person may be in.
On the other hands, some concepts that are not dealing with emotions may also take long. For example, perhaps someone wants to change their career to something that makes them feel fulfilled. This can take months to years to fully bring into fruition, and the goal may change along the way – perhaps one job stops bringing a person fulfilment, so they continue to search for their passion.
Regardless of the circumstance, integration should not be rushed. It may take a couple of minutes to a few years – the important thing to know is that integration is not a race. Just like regular psychotherapy can be a lifelong journey for many, so is integration. Not to mention that if a person partakes in more psychedelic trips while they are integrating an older trip, this can shift their integration journey as new goals and insights are brought to the surface.
The Benefits of Psychedelic Integration Therapy
- Process Feelings of Depression: Psychedelic experiences may show people insights into their state of mind that can be verbalized to a therapist; this can in turn open up the opportunity to treat depression by combining psychedelic experiences with talk therapy.
- Increased Self-Awareness: Psychedelic experiences can provide profound insights into one’s inner self and life’s complexities. Integration therapy helps individuals process these insights, leading to increased self-awareness and personal growth.
- Improved Relationships: As individuals gain clarity about their emotions and experiences during integration therapy, they often experience an improvement in their relationships with others.
- Addiction Recovery: Psychedelic integration therapy has shown promise in helping individuals with substance use disorders find new perspectives and motivations for recovery.
- Spiritual Growth: For many individuals, psychedelic experiences have a spiritual dimension. Integration therapy can help individuals navigate and make sense of these spiritual insights, leading to a deeper sense of connection and purpose.
- Increased Creativity: People may find a newfound sense of creativity after undergoing a psychedelic trip. Integration can help people step into this new creative energy by promoting creating art or music.
Is Psychedelic Integration Therapy Important?
Absolutely. Psychedelic integration is a vital part of any psychedelic experience and should not be skipped . It is a practice that can help transform conceptual ideas into real, tangible change.
Psychedelics will show new facets of a person and ways that they can improve their life. Without partaking in psychedelic integration, then a person is only seeing the potential they have and is doing nothing to try and reach said potential. Psychedelics can show a person where they can be, but that is it – it only shows, it does not change anything. The change has to come from the person who is willing to put in the work and take steps to make that change.
Integration is simply the process of going from where a person was to where they want to be . It helps move them to a new, better destination, if they choose to walk down that road. Without participating in integration work, a person is willingly choosing to simply sit in the middle of the road of life and see opportunities pass them by; without integration, there is no way to create the long-lasting change that a person may be seeking from psychedelics.
Psychedelic integration therapy is a powerful, essential tool that can maximize the therapeutic benefits of psychedelic experiences. By providing a safe and supportive space for individuals to process their journeys, integration therapy helps unlock the transformative potential of these substances. As the field of psychedelic research continues to evolve, integration therapy is expected to play an increasingly essential role in facilitating personal growth, healing, and self-discovery. It is important to remember that integration is not an optional part of a psychedelic journey, but rather a way to help bring the insights of the journey into fruition and help them cause tangible, impactful change in one’s life.
Leave a Reply
Your email address will not be published. Required fields are marked *
Related News

Unmasking Fake Acid: The Dangers of 25I-NBOMe Disguised as LSD

Octopuses On MDMA Want to Snuggle Just Like You

Africa’s Forgotten Cradle of Psychoactive Plants – Global Psychoactive Plant Use Research
Psychedelic Spotlight is your reliable source for the latest stories in the emerging psychedelics industry, covering breakthrough discoveries, investor news and cultural reform.
- Advertise With Us
- Privacy Policy
- Terms and Conditions
- Conferences
Get a roundup of Psychedelic news stories in your inbox
By signing up to the Psychedelic Spotlight newsletter you agree to receive electronic communications from Psychedelic Spotlight that may sometimes include advertisements or sponsored content.
Click to download our Free Psilocybin Sourcing Guide
A First-Timer’s Guide to Psychedelic Mushroom Therapy
Have you ever heard the phrase “turn on, tune in, drop out?” If you are new to the realm of psychedelia, that phrase may mean nothing to you. In the 1960s, Timothy Leary—psychologist and drug advocate—coined that phrase, defining and encompassing a generation in less than 10 words.
“Turn on” tells us to feel deeply. “Tune in” refers to a way of harmonizing with the natural world. “Drop out” heralds this idea of exiting society. The phrase undoubtedly evokes images of psychedelics, and while we don’t condone dropping out of society entirely (necessarily), there is one certainty: psychedelics profoundly shift your general state of awareness in life.
When it comes to psychedelic therapy , it may feel like a daunting or intimidating process trying to curate an ideal therapeutic psychedelic experience, but the benefits are beyond rewarding.
In this beginner’s guide, we’ll explore everything you need to know about this fascinating and rapidly-evolving field of therapy in five steps, so that you have a quick and easy direction toward a transformative experience.
We will cover topics like: how to prepare for a session, what to expect during a psychedelic experience, and how to integrate insights and experiences gained during the journey into daily life.
#1: What Is Psychedelic Therapy?
Psychedelic therapy refers to the therapeutic use of psychoactive substances to facilitate psychological healing and personal growth. It has gained popularity in recent years due to its potential to help people access deeper states of consciousness, which can lead to profound insights, emotional breakthroughs, and a greater sense of connection.
There are quite a few health conditions that psychedelics can treat —all proven by recent research, and psychedelics not only affect the brain but also various bodily systems and processes.
In a past article, we discussed the differences between therapists and guides , but we will summarize the general idea here for you. While the term therapy usually applies to the practice of a licensed therapist, this word is evolving as new forms of treatment and facilitation are emerging.
Given the current legal state of psychedelics in the US—being that they are still classed as Schedule I under the Controlled Substances Act of 1970–psychedelic therapy with a licensed therapist is not really an option for most people.
However, because psychedelic state laws are beginning to change—such as those in Oregon and Colorado which have allowed for regulated psychedelic therapy in the state—the term therapy will likely be the most obvious label.
But for the sake of this article, we will refer to our services as intentional psychedelic experiences, and the guides that we work with will be referred to either as guides or facilitators.
While a therapist is a trained and licensed mental health professional, a guide or facilitator is someone who has extensive experience with psychedelics and aids others in navigating the complex terrain of their trip. To ensure a safe and effective journey, facilitators offer technical support around preparing for a psychedelic experience, the experience itself, and integration.
Psychedelic therapy works by creating a safe and supportive environment for the individual to explore their inner experiences and emotions, and when intense emotions arise, someone is there to help keep you calm and secure.
The benefits of psychedelic therapy are numerous. Research has shown that it can be effective in treating depression, anxiety, and addiction, and can lead to a greater sense of well-being and life satisfaction. It can also facilitate spiritual growth, enhance creativity , and increase empathy and social connection.
#2: Make a Few Decisions For Your Psychedelic Journey
Before embarking on a psychedelic therapy journey, it is important to make a few key decisions to lay the groundwork for your overall experience. Here at Psychedelic Passage, we connect psychedelic seekers with a network of pre-vetted psychedelic facilitators for your intentional, guided journey.
We encourage you to book a consultation with us today to get connected with our network of guides and to help you decide whether or not this form of treatment is right for you.
When it comes to psychoactive substances, the set and setting is crucial in determining the quality of your experience. It is important to choose a facilitator who is experienced, trustworthy, and that you resonate with.
So the first decision to make is which facilitator is right for you. During this process, you will undergo a health screening to ensure that you are physically and mentally healthy enough to participate in the therapy.
The second decision is regarding which substance you prefer and sourcing it safely to avoid drugs that have been doctored up with potentially harmful additives. Once you have sourced, using a drug testing kit can be helpful.
Different substances have unique effects on the body and mind, and it is important to choose one that aligns with your goals and intentions for the experience. The facilitators work with clients interested in psilocybin (magic) mushrooms, MDMA, LSD, ketamine, cannabis, DMT, and mescaline, although shrooms are the most common choice.
The location and setting is another important decision to make, being sure to choose a location that is comfortable, safe, and conducive to relaxation and introspection. Will you travel or do you prefer to be closer to home? Do you want to be in a rental near where you live or in your actual home? These are things you need to consider and decide when planning out the journey.
In a past article, we explored the differences of having mind-altering experience while on a psychedelic retreat versus a one-on-one experience , and we als covered how much psychedelic therapy costs .
#3: Prepare For The Psychedelic Experience
We created a step-by-step guide for preparation leading up to a psychedelic session, but here are some key points to consider:
Educate yourself on the appropriate dosage and storage of the substance in question. Certain substances require different dosages, and it is important to ensure that the substance is stored safely to prevent contamination or degradation.
It is also important to know the risks and potential side effects of the substance, and even know how to take therapeutic psychedelics —because there are multiple ways to ingest them.
Mental and emotional preparation is also crucial in ensuring a positive experience. This can involve setting intentions for the journey and cultivating a sense of openness and curiosity through meditation.
It is important to approach the experience with respect and reverence, and to acknowledge that the journey may bring up challenging emotions or experiences. Some people even follow a special diet leading up to the day. We even have a guide on how to talk to your healthcare provider about psychedelics and your interest in them.
Lastly, prepare your space by maybe setting up a comfortable and calming physical space, with dim lighting, comfortable seating, and choosing a music playlist.
#4: Know What to Expect For The Trip Itself
When embarking on a psychedelic therapy experience, it is important to have a basic understanding of what to expect. Depending on the psychoactive drug, the experience typically involves several different stages, including the launch, peak, and descent.
The come-up can be gradual or drastic, and can involve physical sensations such as nausea, increased heart rate, and sweating. The peak is often characterized by intense sensory experiences and profound emotional and psychological insights, while the come-down can involve a gradual return to baseline, often accompanied by feelings of gratitude and awe.
Along with physical sensations, the psychedelic experience can also bring up a range of emotional sensations, including euphoria, fear, anxiety, and sadness, joy, gratitude, contentment, or paranoia. Surrendering to the experience can help you broaden your capacity to handle intense emotions and sensations.
It is also important to be prepared for the possibility of challenging experiences or “ bad trips .” Having a psychedelic guide, however, can help mitigate some of the risks associated with bad trips and increase your likelihood of having a positive yet meaningful experience.
#5: Integrate The Mind-Altering Experience
Firstly, it is important to prioritize rest and recovery following a psychedelic therapy session. The experience can be physically and emotionally taxing on the body and the mind. Continuing self-care practices like exercise, healthy eating, practicing self-compassion, yoga, meditation, and introspection allow space for your processing.
While integration will be more important for certain people, especially those who have a past history of trauma or just had a stressful or intense experience, there are benefits in this practice for everyone.
Integration also helps continue that feeling of support and community, so this can extend beyond the scope of the facilitator into talk therapy with a licensed therapist or even trusted and neutral family members or friends.
Follow-up sessions with the facilitator are an integral part of the psychedelic journey, but other aspects of integration would include self-reflection, journaling, and finding supportive community.

Talk to a Psychedelic Professional
We at Psychedelic Passage aim to provide in depth resources, articles, and information on psychedelic topics ranging from scientific research to helpful guides and tips.
Visit our resources page to discover more, and if you are interested in a facilitated psychedelic journey, please book a consultation with us. We would love to support you through your experience, and thanks for reading!
Frequently Asked Questions About Psychedelic Mushroom Therapy
How does psychedelic-assisted therapy work.
A therapeutic approach to psychedelic usage, or specifically psilocybin-assisted therapy, involves medicinally using psilocybin or other psychedelic substances for therapeutic benefits with a guide.
Psychedelic facilitators or guides provide general support during a trip as well as support around preparation and integration and tips, tools, and resources for having a safe and meaningful experience.
Because these experiences can be deeply introspective and profound, having a guide can help you gain further insights, process emotions, and potentially find resolution to psychological or emotional challenges.
What conditions or disorders can psychedelic mushroom therapy treat?
Psychedelic mushroom therapy has shown promise in the treatment of various mental health conditions and disorders. Some of the conditions that have been explored include:
- Treatment-resistant depression
- Anxiety disorders , such as generalized anxiety disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD)
- Addiction , including alcohol and tobacco addiction
- Existential distress in patients with life-threatening illnesses , such as cancer
- Obsessive-compulsive disorder (OCD)
- Cluster headaches (also known as “suicide headaches”)
Is psychedelic mushroom therapy safe?
Psychedelic mushroom therapy, when conducted in a controlled and supervised therapeutic setting, has generally demonstrated a good safety profile. There are a few factors that contribute to the safety of a psychedelic trip:
- Set and setting: The mindset and environment in which psychedelic therapy takes place are crucial. A supportive, comfortable, and emotionally safe setting with trained professionals can minimize the risk of adverse experiences.
- Patient screening: Thorough medical and psychological screening processes help identify individuals who may be at risk for potential complications or adverse reactions.
- Professional guidance: Having experienced therapists or facilitators present during the therapy sessions ensures proper support, guidance, and safety monitoring throughout the experience.
Looking for a professionally supported in-person psychedelic experience?
Take the first step and book a consultation call with us today. We'll walk you through every step of the process after getting to know you and your unique situation.
Related posts
How do psychedelics affect your sex life and performance.
The intentional use of psychedelics has been on the rise—primarily for treating conditions like PTSD, anxiety, and depression. But what about their potential effect on
From Addiction to Sobriety with Psychedelic Therapy Ft. Vanessa Crites
This article is inspired by our insightful podcast episode hosted by Psychedelic Passage co-founder, Jimmy Nguyen, which you can listen to on all streaming platforms.
At Psychedelic Passage, we offer professional 1-on-1 guidance and companionship on your journey of healing. We simply can't sit back and let Americans continue to sit in silent suffering trying to battle mental health issues within a broken health care system, all while knowing that effective alternatives exist. We stand for the sacred, at-home, ceremonial use of psychedelics for consciousness exploration, which we believe to be a fundamental human right.
Everything you need to know about how our service works
See the questions most of our clients ask
All you need for proper preparation, integration and ceremony
Sign up for our newsletter and get our free psilocybin sourcing guide
We only send you what you need to know to use psychedelics for your healing journey.
- Website by SQ & TWD
- Privacy Policy
- Terms of Use
- © Psychedelic Passage. All rights reserved
DISCLAIMER: Psychedelic Passage does not provide psychoactive or controlled substances. Many controlled substances are illegal. The illegal use of a controlled substance may result in criminal consequences. Using controlled substances outside of the lawful supervision of a medical professional may also result in serious health complications including death. We are not licensed therapists, counselors, or medical professionals. We are not spiritual guides or scientists. We are a harm reduction company. Please use your discretion and consult a medical professional to ensure our services meet your needs. Any referrals to third parties that we may provide are informational, for your convenience only, and based on the criteria you provide to us. You are solely responsible for making a selection of a practitioner or other service and determining whether he/she/they are appropriate for you. No referral is an endorsement or recommendation of the practitioner or their services. Please conduct your due diligence on any practitioner you use. We do not provide referrals to “underground” (illegal) psychedelic services. Any information received through our services should be considered for educational purposes and not be misconstrued as medical or legal advice. Please use your discretion and consult with a medical professional to ensure our services meet your needs.
13918 E. Mississippi Ave. #68175 Aurora, CO 80012
Search for anything like: microdosing, dosage, integration
Download Our Free Psilocybin Sourcing Guide!
For harm-reduction purposes, we provide links to online psilocybin vendors, local stores, delivery services, and spore vendors for growing your own medicine at home.
Congratulations! We've sent the sourcing guide to your inbox.
You can now close this window.
Get Your Free Psilocybin Sourcing Guide!
Just tell us where to send it…
How psychedelic-assisted therapies can be more effective
A new study of psilocybin patients zeroes in on a crucial element of treatment.
By Mack DeGeurin | Published Apr 23, 2024 2:37 PM EDT

In just a few short years, psychedelic-assisted therapy involving controlled substances like ketamine, MDMA, and psilocybin (the psychoactive compound found in “magic mushrooms”) have evolved from relative obscurity to the far edges of mainstream medical acceptance . Clinical studies have shown that their medical use can have positive effects for patients living with depression and post-traumatic stress disorder . Sometimes, these treatments prove effective where other, more widely-prescribed medications fall short . But new research suggests close bonds with a trained therapist is a key element contributing to effective psychedelic-assisted treatment, specifically psilocybin.
[Related: 4 visionaries on the history and future of psychedelic medicine ]
A surge in interest in therapeutic use of psychedelics has fostered a burgeoning industry of startups specializing in treatments. As of today, according to the psychedelics industry tracker Psilocybin Alpha, more than 50 publicly traded companies currently offer psychedelic therapy (mostly ketamine) and psychedelic retreats. Yet, the exact ways these companies administer psychedelics can vary widely. While some require patients to consume or inject the substance in the presence of a trained clinician, others lean on loose, pandemic-era health regulations to let patients take the medication at home , typically as pills and lozenges. The latter method can carry risks. In some cases, the Federal Drug Administration, which has yet to approve psychedelic drugs for therapy, claims it has received reports of patients experiencing adverse health effects after they’ve taken medically prescribed ketamine at home without a clinician’s supervision. There are currently no legal at-home psilocybin treatments available however individuals in Oregon were able to begin accessing the compound without a prescription last year.
A new study published in the journal PLOS ONE this week suggests that strong relationships between patients and their therapists could play a crucial role determining whether or not psychedelic-assisted therapy can prove useful as treatments for depression. The study, which analyzed a 2021 clinical study involving 24 patients using psilocybin-assisted therapy to treat severe depression, found that participants with stronger self-reported connections with their therapist were more likely to report a decrease in depression over time.
In other words, the efficacy of psilocybin treatment increases over the long-term when a patient feels more connected to their clinician. The clinician provides hours or preparation and also guides the patient through the experience and dissects it days and weeks later. Findings like these could help influence treatment standards for psychedelic-assisted therapy treatments, especially as the practice gains more widespread clinical acceptance and adoption.
Patients with stronger connections to their therapists reported better results
Researchers from Ohio State University examined data from a 2021 clinical trial where 24 adults seeking treatment for severe depression received two doses of psilocybin paired with 11 hours of psychotherapy. Patients completed survey questionnaires where they assessed the strength of the relationship with their therapists, which the researchers refer to as their “therapeutic alliance.” The patients also noted down any mystical or insightful psychological experience they had during the treatment. Researchers say at times these experiences tend to yield positive therapeutic outcomes, particularly in the short and medium term. In this case, these experiences led to positive outcomes around four-weeks after introducing the psilocybin into treatment.
Higher alliance scores, or stronger relationships with therapists, correlated with longer-term psychological insights. One year after the treatments, patients who reported strong connections with their therapist also crucially provided lower self-reported depression scores one year following treatment than those who reported weaker relationships. The research builds off of past studies that show how a strong therapeutic alliance between a therapist and a patient often leads to a more effective outcome following therapy. This new study suggests those same basic findings similarly apply to psychedelic-assisted therapy.
“This concept is not novel. What is novel is that very few people have explored this concept as part of psychedelic-assisted therapy,” paper senior author and Center for Psychedelic Drug Research and Education associate professor Alan Davis said in a statement. “This data suggests that psychedelic-assisted therapy relies heavily on the therapeutic alliance, just like any other treatment.”
The findings also reinforce the role a patient’s environment and mindset, known colloquially as “set and setting” can have on influencing positive experiences. In this case, hours of preparatory psychotherapy prior to administering psilocybin, along with “supportive, no direct” therapy during the actual psychedelic experience posed to be significant variables contributing to the drug’s overall effectiveness. Patients who were more comfortable with their clinician may be more receptive to the therapy.
“That’s why I think the relationship has been shown to be impactful in this analysis–because, really, the whole intervention is designed for us to establish the trust and rapport that’s needed for someone to go into an alternative consciousness safely,” Davis added.
The study’s findings come during what could be an inflection point for psychedelic-assisted therapy research and treatment in the US. Despite still being labeled a Schedule 1 drug on the national level, several cities including Denver, Oakland, and Washington have decriminalized psilocybin. On the medical front, the FDA in 2019 approved the use of a nasal spray called Spravato , which uses a derivative of ketamine, for treating depression. Just last year, the FDA released its first-ever draft guidance outlining considerations for researchers looking to conduct clinical trials for psychedelic treatments. An MDMA therapy from the MAPS Public Benefit Corporation could reportedly receive FDA approval by the end of the year .
Ohio State University College of Medicine resident and paper lead author Adam Levin notes he and his fellow researchers’ findings could highlight the importance of maintaining strong connections between patients and physicians, especially with treatments posed to gain wider adoption in the coming years. Levin, and others critical of attempts to rush out access to psychedelic drugs without proper therapeutic support warn such an approach could lead to unintended consequences and even set back efforts to make psychedelic-assisted therapy more widely available.
“Our concern is that any effort to minimize therapeutic support could lead to safety concerns or adverse events,” Levin said. “…What we showed in this study is evidence for the importance of the alliance in not just preventing those types of events, but also in optimizing therapeutic outcomes.”
Like science, tech, and DIY projects?
Sign up to receive Popular Science's emails and get the highlights.
- Share full article
Advertisement
Supported by
What Does Good Psychedelic Therapy Look Like?
As MDMA and psilocybin treatments become more mainstream, the therapy component has come under scrutiny. Here’s what’s common in many sessions — and what’s not.

By Dana G. Smith
Psychedelic therapy is on its way to becoming a mainstream medical treatment in mental health care. In 2020 and 2022, residents of Oregon and Colorado voted to legalize the use of psilocybin, the psychoactive ingredient in hallucinogenic mushrooms, and the Food and Drug Administration is expected to approve it and MDMA, or Ecstasy, to treat depression and post-traumatic stress disorder by 2024.
While there is mounting evidence that psychedelics could offer much-needed new treatments for intractable mental illness, stories of abuse or trauma have also emerged — which have more to do with the therapists than the drugs.
Some cases involve clear instances of sexual assault. With others, the therapist may have had good intentions but still caused more harm than healing. In one recent clinical trial , which found that psilocybin could offer relief for treatment-resistant depression, three participants reported having suicidal thoughts and harming themselves in the weeks following the therapy.
Twenty years of research has standardized the dosage of the drugs used in clinical trials, but the therapy part has not received similar scrutiny. Instead, therapists’ work is often based on tradition rather than empirical evidence, said Dr. Charles Raison, the director of clinical and translational research at the Usona Institute in Wisconsin and a professor of psychiatry at the University of Wisconsin.
The lack of scientifically backed best practices has prompted researchers, clinicians and former patients to call for a more critical look at the therapeutic component of psychedelic therapy.
“I’m really concerned about the ways in which well-meaning therapists can do harm,” said Sarah McNamee, a licensed psychotherapist and research coordinator at the School of Social Work at McGill University.
Because people are so emotionally vulnerable while they’re on psychedelics, there is a greater risk for psychological injury, particularly by inept or inexperienced practitioners. “It could be easy to make someone worse,” said Janis Phelps, director of the Center for Psychedelic Therapies and Research at the California Institute of Integral Studies, which offers degrees in psychology and counseling.
Here’s what currently happens in many psychedelic therapy sessions, and where red flags might appear.
Choosing a therapist
In most of the country, the only way to legally try psychedelic therapy using psilocybin or MDMA is to enroll in a clinical trial . (Ketamine can be administered in clinics or can even be sent to your home, but the experts strongly urge that it be used only in conjunction with therapy.)
The practitioner you work with should be a mental health professional, ideally specializing in your condition, and certified in psychedelic therapy, for which there are now several training programs . Amy Lehrner, the clinical director of the Center for Psychedelic Psychotherapy and Trauma Research at the Icahn School of Medicine at Mount Sinai, recommended that people assess a potential psychedelic therapist as they would any other mental health provider: Ask about the person’s training, professional certifications and expertise.
Underground options have also existed for decades, some administered by professional therapists, others by amateurs. Experts advise against using such providers because there is even less oversight. Vetting the practitioner is doubly important if you are seeking psychedelic therapy outside a clinical trial.
In any setting, it is crucial that you feel safe and comfortable with the therapist, which is one reason that preparatory sessions are so important for developing trust and rapport.
Preparatory sessions
Before you take the drug, the clinician should meet with you for several hours over a few days to explain what the treatment will entail, especially regarding the drug’s physical and psychological effects. The therapist should ask about your history and symptoms, as well as your goals and intentions for the treatment.
The therapist might advise you to adopt a certain frame of mind during the session or teach you breathing or meditation techniques to use if you are faced with an uncomfortable emotion or physical sensation while on the drug.
“We teach them to be excited and curious about what they don’t know yet, what’s going to come out of them, and to welcome it, even if it’s disturbing for a few moments — or an hour, if that’s the case,” Dr. Phelps said.
A critical purpose of these sessions is to obtain informed consent for what might happen during the drug session, especially regarding touch. Because it is not normally part of talk therapy, the role of touch in psychedelic therapy is contentious .
Some experts say that it can be helpful for someone on a psychedelic trip to receive a reassuring touch. Others say it could create an opportunity for boundaries to be crossed. Most agreed that the touch should be limited to holding hands or a hand on the shoulder; anything involving full-body contact, including a hug, could be interpreted as sexual.
Drug session
For most of a drug session with MDMA or psilocybin, the patient is typically lying down, eyes closed, listening to music. The experience generally does not involve much talking and is more internal for the patient.
If the patient starts to feel anxious or is encountering a traumatic memory or vision, the therapist might offer reassurance or guidance through a breathing exercise. In those instances, the goal is not for the patient to avoid or be distracted from the experience. “The therapist role here is to try to help people stay with it,” Dr. Raison said. “If you fight the experience, you tend to have bad outcomes.”
Therapists should never push a certain experience on a patient; they are there to follow the patient’s direction, not to lead, Dr. Lehrner said. “It is never about intruding or directing by pushing somebody” past their limits.
However, Ms. McNamee, who has participated in psychedelic clinical trials, said that uncritically encouraging patients to go through the pain could cause more harm than good. In psychedelic therapy, therapists often push people “to confront the distress,” she said, when sometimes “it might be a good idea to turn away from distress, to soothe, to regulate, to distract.”
It’s not about whether a practice is good or bad, she added, but determining in what contexts it can be helpful or harmful.
Integration sessions
The integration sessions, when the patient processes the experience in the days and weeks after the trip, look the most like traditional therapy. The exact number of sessions varies, but four hours spread over two or three weeks is typical, though some experts say that isn’t long enough.
The therapist helps the patient try to make sense of the feelings, insights and memories that emerged while on the psychedelic. The most common tactic, Dr. Raison said, is to ask open-ended questions and let the patient guide the conversation.
For example, a therapist might ask: How did the experience shift your relationship with yourself? The goal is to take those lessons and incorporate them into the patient’s life, the philosophy being that “the patient has their own wisdom, the psychedelic experience has its own wisdom,” he said.
Some researchers are starting to experiment with alternative therapeutic approaches , such as cognitive behavioral therapy or acceptance and commitment therapy , that encourage patients to re-examine beliefs about themselves, potentially aided by insights made during the psychedelic session.
To Dr. Lehrner, what researchers should be working to standardize now are general therapeutic principles while they continue testing whether the treatment as a whole is safe and effective. “Afterwards,” she said, “people may investigate: ‘Well, what if we tweak it like this? What if we change it like that?’”
Ms. McNamee disagreed. “I worry about how the field might be moving too quickly,” without sufficient research into what constitutes safe and ethical practice, she said. “That we may standardize things that are problematic, I think, is something that’s worth thinking about.”
Dana G. Smith is a Times reporter covering personal health, particularly aging and brain health. More about Dana G. Smith
Advances in Psychedelic Therapy
Psychedelics — though mostly still illegal — have surged in popularity in recent years as alternative treatments for mental health..
After decades of demonization and criminalization, psychedelic drugs are on the cusp of entering mainstream psychiatry , with U.S. combat veterans leading the lobbying effort .
Psychoactive mushrooms, legal in Oregon but still illegal under federal law, are gaining popularity as therapy tools .
As psychedelics move from the underground to mainstream medicine, clinicians aspiring to work in the field are inducing altered states with deep breathing .
MDMA-assisted therapy , which seems to be effective in reducing symptoms of post-traumatic stress disorder, is inching closer to approval in the United States .
Ketamine has become increasingly popular as a therapy for treatment-resistant depression . But the misuse of the anesthetic drug has spurred F.D.A. warnings .
Many drugs known for mind-altering trips are being studied to treat depression, substance use and other disorders. This is what researchers have learned so far .
While psychedelics are showing real promise for therapeutic use, they can be dangerous for some. Here’s what to know about who should be cautious .
Celebrating 25 Years
- Join ADDitude
- |

- What Is ADHD?
- The ADHD Brain
- ADHD Symptoms
- ADHD in Children
- ADHD in Adults
- ADHD in Women
- Find ADHD Specialists
- New! Symptom Checker
- ADHD Symptom Tests
- All Symptom Tests
- More in Mental Health
- Medication Reviews
- ADHD Medications
- Natural Remedies
- ADHD Therapies
- Managing Treatment
- Treating Your Child
- Behavior & Discipline
- School & Learning
- Teens with ADHD
- Positive Parenting
- Schedules & Routines
- Organizing Your Child
- Health & Nutrition
- More on ADHD Parenting
- Do I Have ADD?
- Getting Things Done
- Relationships
- Time & Productivity
- Organization
- Health & Nutrition
- More for ADHD Adults
- Free Webinars
- Free Downloads
- ADHD Videos
- ADHD Directory
- eBooks + More
- Newsletters
- Guest Blogs
- News & Research
- For Clinicians
- For Educators
- Manage My Subscription
- Get Back Issues
- Digital Magazine
- Gift Subscription
- Renew My Subscription
- ADHD Medication & Treatment
“How a Psychedelic Trip Changed My Life”
A psychedelic trip on magic mushrooms led me to embrace my neurodiversity, and now, i help others do the same as a psychedelic-assisted therapy facilitator..

Twelve years ago, I embarked on a transformative psychedelics journey that opened my eyes to my true self. I did not know then that this trip into my subconscious would completely change my perception of the world, make my then- undiagnosed ADHD more manageable, and lead me to help others experience similar life-changing revelations.
On that fateful day, my psychedelic guide gave me magic mushrooms and said, “Look at the forest one last time; you will never see it the same way again.”
To say he was right would be an understatement.
I arrived with a simple intention: to get to know myself better. What emerged were aspects of myself that I never knew existed. The psychedelic experience revealed the roots of my depression and provided insight about how to regulate my emotions — a godsend for me as I struggled with intense mood swings and disorders. Whereas therapy had failed, this journey transformed me entirely.
To be clear, it was not a magical solution that solved all my problems overnight. But my psychedelic journey gave me a vision of the destination to drive toward. It filled me with an intrinsic motivation to change the patterns that were keeping me stuck.
[ Read: The Truth About Lion’s Mane, Psychedelics & Caffeine ]
Fast-forward 12 years, following numerous psychedelic experiences combined with therapy: I have achieved a state of emotional stability. Severe mood swings and depression are a distant memory.
I was diagnosed with ADHD last year, and I consider this revelation the last missing piece of my puzzle. Today, I find it easy to love myself for who I am. I have developed new ways to live and embrace my ADHD brain without using medication.
Helping Others Follow the White Rabbit
In 2016, I decided that I wanted to help others by becoming a psychedelic-assisted therapy facilitator. At the time, psychedelic facilitator training programs didn’t exist, so I pursued extensive training in various modalities. I trained in inner child work and trauma integration therapy. I attended workshops and seminars conducted by experts in the field of psychedelic-assisted therapy.
Since then, I have co-founded a psychedelic-assisted therapy company and guided hundreds of people through psilocybin journeys in the Netherlands, where this work is legal. The changes I have witnessed in people, especially those with ADHD and neurodiversity, have been nothing short of astounding.
[ From WebMD: A Long, Strange Trip — Psychedelics Meet Mainstream Medicine ]
Most of the people undergoing this form of therapy experience significant changes in their lives, overcome addictions and depression, transform their self-doubt , and reduce their rejection sensitivity .
It is important to say that this therapy is not for everyone, nor is it a one-size-fits-all solution. Individuals who are prone to psychosis, diagnosed with schizophrenia or bipolar disorder , or who have a family history of these conditions should abstain from this therapy.
That said, it helped me to redefine my life, and I hope it can benefit others like me.
Psychedelic Assisted Therapy: Next Steps
- Free Download: Free Guide to the Top 5 Vitamins and Supplements for ADHD
- Read: LSD, MDMA, Magic Mushrooms Clinical Trial Guidelines Released by FDA
- Read: Real Stories of Using Ketamine for Depression, Anxiety, PTSD
- Read: “Therapy Helped Me…”
Alice Smeets is a neurodivergent psilocybin-assisted therapy facilitator and co-founder of A Whole New High , which offers guided, private psilocybin therapy sessions and group retreats in the Netherlands.
SUPPORT ADDITUDE Thank you for reading ADDitude. To support our mission of providing ADHD education and support, please consider subscribing . Your readership and support help make our content and outreach possible. Thank you.
ADHD Therapies: Read These Next

Right Goal, Wrong Strategy — 11 New Treatment Ideas

Treatments for Depression and ADHD: New and Forthcoming Approaches

ADHD Therapy Overview: The 9 Best Treatments for Children and Adults

Somatic Therapy: Understanding the ADHD Brain, Body & Trauma
Adhd newsletter, treating adhd, food and nutrition, medication, supplements, natural therapies, and more..
It appears JavaScript is disabled in your browser. Please enable JavaScript and refresh the page in order to complete this form.

9 Conditions Often Diagnosed with ADHD
What is the Best Music for a Therapeutic Psychedelic Trip?
What is the best music for a therapeutic psychedelic trip music can play an essential role in supporting mystical experiences and insights..
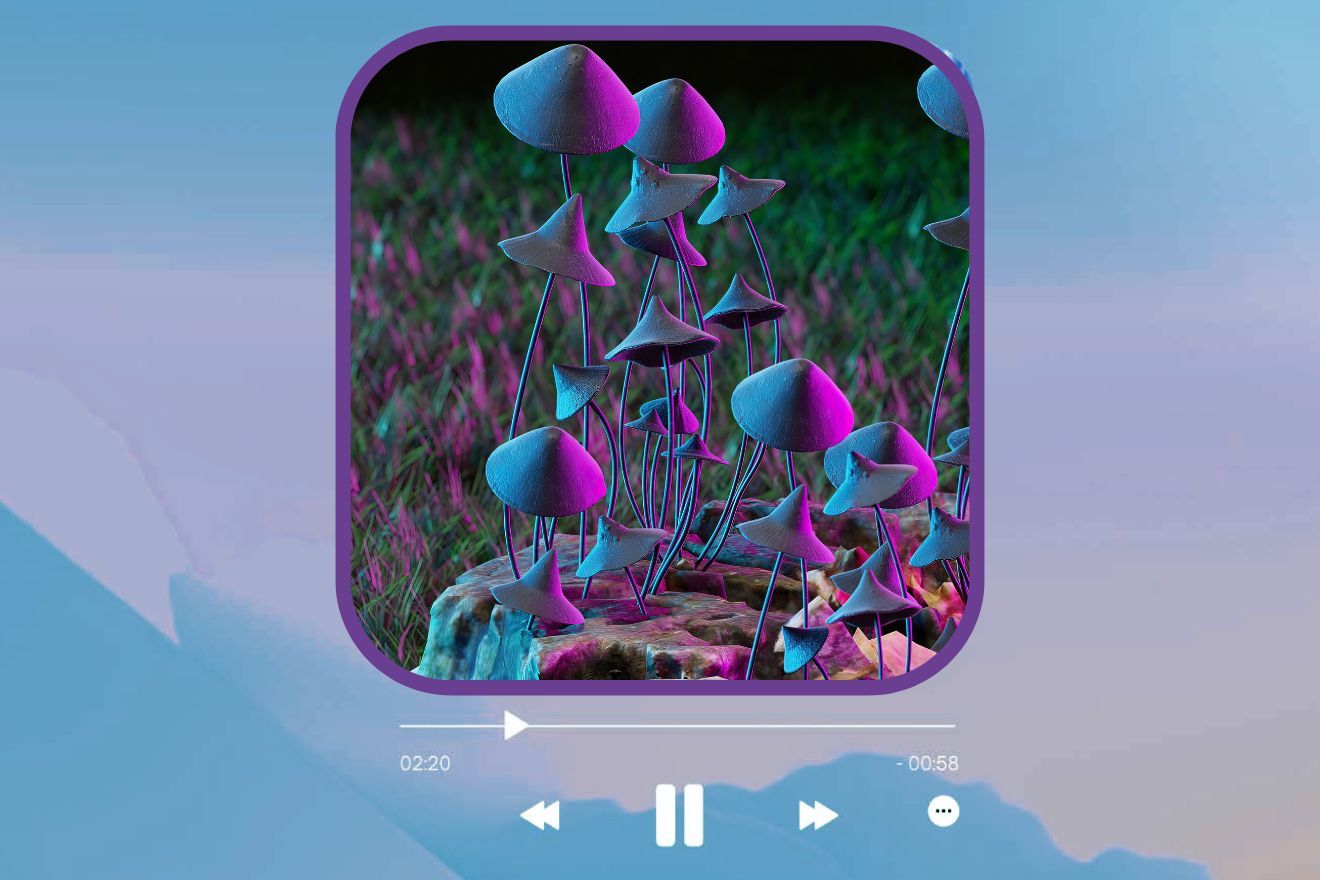
Many consider music to be core to the psychedelic experience. Going back millennia, music features prominently in the indigenous use of psychedelics (such as the rattle and drum used in peyote ceremonies and the icaros , or traditional indigenous Amazonian songs, performed in ayahuasca ceremonies). In a Western context, by the late 1950s, music’s important contribution to psychedelic therapy was firmly established.
Stephen Lett and Erika Dyck write in a paper published in the journal Social History of Medicine that “religious sounds and music were both incorporated into and strategically avoided in the early psychedelic therapeutic sessions in an effort to achieve spiritual epiphanies at peak experiences” [1].
Since the 1950s, music has remained a staple of psychedelic-assisted therapy. It has been deemed so important that in a 1961 article , a team of researchers studying the effects of LSD on alcoholism and other psychiatric problems stated, “We think a group of four [therapists] is best. Generally, this includes the psychiatrist (as therapist), a psychologist (co-therapist), a psychiatric nurse and a music therapist” [2]. They recognized, in other words, the need for professional expertise with respect to the therapeutic use of music in psychedelic sessions.
But the question arises: What music should you listen to during a psychedelic session? Should you listen to one particular type of music in order to achieve spiritual or peak experiences? As Lett asks in an article for Chacruna : “Is it music’s emotional content or a patient’s familiarity with music that most reliably led to the desired outcome?” Of course, the answers to these questions are relevant for all kinds of psychedelic use, not just clinical, supervised sessions. Fortunately, researchers are beginning to shed some light on this topic.
The History of Music Selection for Psychedelic Therapy
In his article for Chacruna, Lett notes how Hermina H. Browne (1902–1966) was one of the first music therapists involved in psychedelic-assisted therapy. She developed a method for selecting music to accompany psychedelic sessions for alcoholics. Browne selected music based on emotional content, as well as the patient’s age, cultural background, and preferences.
In a later study, she chose music based on mood, quality, familiarity, general suitability, and the subject’s requests based on these criteria. Midway through the study, Browne devised a structured presentation of music, playing a particular ‘category’ of music for each period of listening (every other 30 minutes, as in the previous study).
This structured presentation of music:
- “relaxing to tense”
- “very tense, disturbed with a purpose”
- “solemn, meditative, self-searching, spiritual”
- “relaxing, spiritual”
- “reconciling, restoration of confidence, feeling of hope and faith”
These categories of music selected were meant to complement the pattern of reactions observed in previous LSD experiments; it was meant to match the ideal trajectory of a psychedelic session. Lett mentions, too, the work of psychiatrist Humphry Osmond (who introduced mescaline to Aldous Huxley), who argued that the most effective music in psychedelic therapy was that which the patient was most familiar with (which many psychonauts would agree with).
Psychedelic researchers Charles T. Eagle, Jr. and E. Thayer Gaston would come to criticize music therapists who selected music for patients because they deemed it ‘profound’, which they argued was merely a subjective opinion and prone to ideology and elitism. Instead, they insisted that the most therapeutically effective music was whatever the patient found familiar, in agreement with Osmond.
Helen L. Bonny (1921–2010) would become one of the most influential music therapists involved in psychedelic therapy. Her research was based on the notion that music’s emotional content, not its familiarity, was of primary importance (although she accepted that a person’s preferences and history with music were relevant variables, nonetheless).
Modern Research on Music in Psychedelic Therapy
In a 2018 paper published in Psychopharmacology , researchers at Imperial College London refer to music as ‘the hidden therapist’ based on its central role in psychedelic therapy [3]. Dr. Sam Gandy has said that “music can create a new form of structure and narrative in the midst of the psychedelic state, helping guide people through their inner ocean of mind.” Music can also help patients through uncertain, turbulent, or challenging experiences.
We can say, then, that in a directive context, music can facilitate immersive, meaningful, emotional, and awe-inspiring journeys, while in a non-directive context, it can play a calming and soothing role, encouraging feelings of safety and openness to the experience – to the information and insights that are arising.

In the 2018 paper, researchers note that music can support the occurrence of mystical and insightful experiences, which have been found to strongly predict beneficial outcomes of psychedelic therapy , such as reductions in depression, anxiety, and neuroticism and increases in openness.
Read more about the role of music in psychedelic-assisted therapy and listen to session playlists in an article written by MAPS researcher Dr. Ilsa Jerome.
What do researchers believe?
So what do researchers believe is the ideal music to listen to on psychedelics for therapeutic purposes? In the early days of psychedelic therapy, Western classical music was commonly selected, but a 2021 study published in the journal ACS Pharmacology and Translational Science calls into question whether this is the best music to use. It suggests that overtone-based music (emphasizing instruments with a strong overtone signature, such as Tibetan singing bowls, gongs, didgeridoo, chimes, bells, sitar, and human voice overtone singing) was associated with more mystical experiences than Western classical music, which until recently have dominated psychedelic therapy playlists [4].
A 2017 survey looked at individuals who had experience administering psilocybin (on a minimum of 50 occasions) in a therapeutic context. The aim of the study was to identify features of music that best supported the occurrence of mystical experiences. The researchers found that music with “regular, predictable, formulaic phrase structure, and orchestration, a feeling of continuous movement and forward motion that slowly builds over time, and lower perceptual brightness when compared to pre peak music” was ideal in this respect [5].
Wavepaths (Get 10% off with coupon code: PSPARTNER10), a company studying and developing music playlists for psychedelic therapy, states in an article:
“Music involving recognizable vocals is better excluded from psychedelic session music playlists, as exposure to language during a psychedelic experience may reduce chances of mystical experiences from occurring. In addition, language in the form of lyrics is likely to be directive in certain ways which may not always be advantageous for the fine tuned nature of psychedelic sessions.”
How about specific tracks?
In terms of specific tracks that researchers found highly effective, Wavepaths underscore that ‘Azure’ by Greg Haines (2012) stands out . It features in Mendel Kaelen’s playlist used in the 2016 psilocybin for depression study carried out by Imperial College London. It occurs around the ‘peak’ timeframe of the psychedelic session (02:34:41). Wavepaths note that the track “exhibits distinct examples of what Hinton & Kirmayer term ‘metabole’ – “a sudden shift in the music which brings about a change in perception from one state to another.”” These shifts fostered a sense of direction, encouraged the release and processing of emotion, and supported the experience of respite and calm. It had both propelling and anchoring effects. The track was especially personal, emotive, transformative, and therapeutic for participants.
‘Azure’ was also one of the only songs that patients specifically mentioned in post-session interviews , owing to its memorable effect. Here are some of those mentions:
“There’s one track [Greg Haines – Azure] that gets really really really intense.”
“[Greg Haines – Azure] I felt like I was sort of the highest I could get, it was like the absolute, the top of everything.”
“[Greg Haines – Azure] just builds and builds. You’re holding on to an extent, you just kind of go up and you’re like ‘ok, where am I? Can I go any further?’”
“[Greg Haines – Azure] really really beautiful, overwhelming, but really peaceful as well.”
Final Thoughts
This kind of research should in no way create a value judgment on an individual’s choice of music for their psychedelic session. Often, one’s favorite music—whatever the genre or mood—creates the most enjoyable, fulfilling, and memorable experience. (On the other hand, even if you normally love listening to death metal or black metal, this doesn’t mean the music will translate well in terms of psychedelic effects.) What modern research does point to, however, is the potential of certain kinds of music to facilitate specific aims—namely, peak experiences, which can have long-lasting positive outcomes.
Follow your Curiosity
- Lett, S., & Dyck, E. (2022). Tune in, Turn on: Religious Music and Spiritual Power in the History of Psychedelic Therapy . Social History of Medicine , hkac057.
- MacLean, J. R., MacDonald, D. C., Byrne, U. P. B., & Hubbard, A. M. (1961). The Use of LSD-25 in the Treatment of Alcoholism and Other Psychiatric Problems . Quarterly Journal of Studies on Alcohol , 22, 34-45.
- Kaelen, M., Giribaldi, B., Raine, J., Evans, L., Timmerman, C., Rodriguez, N., Roseman, L., Feilding, A., Nutt, D., & Carhart-Harris, R. (2018). The hidden therapist: evidence for a central role of music in psychedelic therapy . Psychopharmacology , 235(2), 505-519.
- Strickland, J. C., Garcia-Romeu, A., & Johnson, M. W. (2021). Set and Setting: A Randomized Study of Different Musical Genres in Supporting Psychedelic Therapy . ACS Pharmacology and Translational Science , 4(2), 472-478.
- Barrett, F. S., Robbins, H., Smoke, D., Brown, J. L., & Griffiths, R. R. (2017). Qualitative and Quantitative Features of Music Reported to Support Peak Mystical Experiences during Psychedelic Therapy Sessions . Frontiers in Psychology , 8, Article: 1238.
- Kaelen, M. (2017). The psychological and human brain effects of music in combination with psychedelic drugs . Doctoral thesis, Imperial College London .
You may also be interested in:

Mental Health

Self-Discovery

Harm Reduction

Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

In psychedelic therapy, clinician-patient bond may matter most
Study links relationship strength to reduced depression for up to 1 year.
Drug effects have dominated the national conversation about psychedelics for medical treatment, but a new study suggests that when it comes to reducing depression with psychedelic-assisted therapy, what matters most is a strong relationship between the therapist and study participant.
Researchers analyzed data from a 2021 clinical trial that found psilocybin (magic mushrooms) combined with psychotherapy in adults was effective at treating major depressive disorder.
Data included depression outcomes and participant reports about their experiences with the drugs and their connection with therapists. Results showed that the stronger the relationship between a participant and clinician – called a therapeutic alliance – the lower the depression scores were one year later.

“What persisted the most was the connection between the therapeutic alliance and long-term outcomes, which indicates the importance of a strong relationship,” said lead author Adam Levin , a psychiatry and behavioral health resident in The Ohio State University College of Medicine .
Past research has consistently found that as mental health treatments changed, a trusting relationship between clients and clinicians has remained key to better outcomes, said senior author Alan Davis , associate professor and director of the Center for Psychedelic Drug Research and Education in The Ohio State University College of Social Work .
“This concept is not novel. What is novel is that very few people have explored this concept as part of psychedelic-assisted therapy,” Davis said. “This data suggests that psychedelic-assisted therapy relies heavily on the therapeutic alliance, just like any other treatment.”
The study was published recently in the journal PLOS ONE .
Twenty-four adults who participated in the trial received two doses of psilocybin and 11 hours of psychotherapy. Participants completed the therapeutic alliance questionnaire, assessing the strength of the therapist-participant relationship, three times: after eight hours of preparation therapy and one week after each psilocybin treatment.

Participants also completed questionnaires about any mystical and psychologically insightful experiences they had during the drug treatment sessions. Their depression symptoms were assessed one week, four weeks, and up to one year after the trial’s end.
The analysis showed that the overall alliance score increased over time and revealed a correlation between a higher alliance score and more acute mystical and/or psychologically insightful experiences from the drug treatment. Acute effects were linked to lower depression at the four-week point after treatment, but were not associated with better depression outcomes a year after the trial.
“The mystical experience, which is something that is most often reported as related to outcome, was not related to the depression scores at 12 months,” Davis said. “We’re not saying this means acute effects aren’t important – psychological insight was still predictive of improvement in the long term. But this does start to situate the importance and meaning of the therapeutic alliance alongside these more well-established effects that people talk about.”
That said, the analysis showed that a stronger relationship during the final therapy preparation session predicted a more mystical and psychologically insightful experience – which in turn was linked to further strengthening the therapeutic alliance.
“That’s why I think the relationship has been shown to be impactful in this analysis – because, really, the whole intervention is designed for us to establish the trust and rapport that’s needed for someone to go into an alternative consciousness safely,” Davis said.
Considering that psychedelics carry a stigma as Schedule I drugs under the Controlled Substances Act , efforts to minimize negative experiences in future studies of their therapeutic potential should be paramount – and therapy is critical to creating a supportive environment for patients, the authors said.
This study ideally will help clearly position psychedelics treatment as a psychotherapeutic intervention moving forward – rather than its primary purpose being administration of a drug, Levin said.
“This isn’t a case where we should try to fit psychedelics into the existing psychiatric paradigm – I think the paradigm should expand to include what we’re learning from psychedelics,” Levin said. “Our concern is that any effort to minimize therapeutic support could lead to safety concerns or adverse events. And what we showed in this study is evidence for the importance of the alliance in not just preventing those types of events, but also in optimizing therapeutic outcomes.”
This work was supported by the Center for Psychedelic and Consciousness Research, funded by the Steven & Alexandra Cohen Foundation, the RiverStyx Foundation and private donors. It was also supported by the Center for Psychedelic Drug Research and Education (CPDRE), funded by anonymous donors.
Additional co-authors are Rafaelle Lancelotta, Nathan Sepeda and Theodore Wagener of Ohio State, and Natalie Gukasyan, Sandeep Nayak, Frederick Barrett and Roland Griffiths of the Center for Psychedelic and Consciousness Research at Johns Hopkins University, where Davis is an affiliate.
More Ohio State News
Administrators share leadership lessons at ohio state forum.
During a recent forum hosted by Ohio State, educators from across the country shared insights on effective leadership.
Social media affects people’s views on mental illness
Even subtle differences in the wording of social media messages may be enough to sway young people’s beliefs about depression and anxiety and their treatment.
A message from President Carter
As the semester draws to a close, I want to thank you for your dedication to teaching, learning, research, patient care – and to Ohio State. As we look forward to spring commencement and the events surrounding this momentous occasion for the class of 2024, I am reminded of the resilience of this class as they navigated starting their collegiate careers during a pandemic.

Contact: Admissions | Webmaster | Page maintained by University Communications
Request an alternate format of this page | Web Services Status | Nondiscrimination notice

Multidisciplinary Association for Psychedelic Studies - MAPS
Psychedelics Today: Updates from MAPS: Current Initiatives, Psychedelic Science 2025, and Music as a Bridge
In this episode, Joe interviews Devon Phillips: Community & Partnerships officer for the Multidisciplinary Association for Psychedelic Studies (MAPS).
Originally appearing here ( Archived )
Download our Integration Guide
Just enter your email in order to download our Integration Guide

Watch CBS News
Push to legalize psychedelic-assisted therapy treatment continues
By Kenny Choi
April 17, 2024 / 7:31 PM PDT / CBS San Francisco
The push to legalize psychedelic-assisted therapy treatments continues, as patients say it helps and the FDA recently said some psychedelic drugs show promise.
Nina Olmstead has struggled with anxiety most of her adult life, but she said her first ketamine assisted therapy session proved to be a breakthrough.
"It gave me a sense of self understanding and self-forgiveness. That is kind of what I was trying to cultivate through therapy," said Olmstead.
Years of traditional therapy and taking anti-anxiety medication didn't work for the Menlo Park resident.
"I've struggled with ADHD. I've just found psychedelic therapies and alternative therapies are a really powerful substitute for those kinds of medications," said Olmstead.
Lawmakers are closer to legalizing psychedelic assisted therapy in California as a new bill is making its way through the state legislature. The effort would expand the types of psychedelic drugs allowed for therapeutic use.
Supporters said this kind of therapy is moving the needle to address mental health struggles.
Lindsay Olshan is a trained psychedelic assisted therapist and founder of FADEN, who leads one-on-one ketamine journeys.
"What we're finding with the psychedelic approach is that people are actually getting into the root cause of a lot of those symptoms and being able to process that fully so that they're not requiring those medicines anymore," said Olshan.
Olshan has cultivated her practice for 20 years. But it was only four years ago when she added psychedelic assisted therapy using Ketamine.
"It deepened people's ability to heal. It enriched the therapeutic process. It gave me more passion for what I'm doing because it really feels like I'm moving the needle with people in a way that has been hard to do," said Olshan.
Prescribed ketamine sessions are legal in California. But the use of psychedelic drugs like hallucinogenic mushrooms and MDMA, commonly known as ecstasy, are not.
State Senator Scott Wiener is trying to change that.
"It's all in the shadows because it's technically a crime, and so our primary goal is to bring it out of the shadows," said Wiener.
Wiener's years-long push to decriminalize the possession of psychedelic drugs came to an abrupt halt with a veto by Governor Newsom last fall.
The revised bill wouldn't make recreational use legal, but rather open the doors for psychedelic assisted therapists.
"We want them to be able to be certified and out in the sunlight and not have to worry about getting arrested. That's really one of our goals here," said Wiener.
The California District Attorneys Association has spoken out against decriminalizing psychedelic drugs so has the California Coalition for Psychedelic Safety and Education, one of the most vocal critics of Wiener's efforts.
It now supports supervised therapeutic use but wants more research and data on psychedelics.
"If it appears that decriminalization of recreational use is appropriate that could happen, but right now the science is just not there and as we've seen use increase, we've seen more adverse events and consequences," said Beth Parker of the California Coalition for Psychedelic Safety and Education.
The new measure, Senate Bill 1012, would require the establishment of a state licensing board that would develop training and oversight rules. Therapists would have to screen individuals.
"I think the impact could be profound in terms of giving people another option to heal and have that be done in a very regulated, safe environment," said Olshan.
"The combination of working with the ketamine and the traditional therapy kind of fused things for me in a way that was really, really impactful," said Olmstead.
For Nina Olmstead, the shift she has experienced, is enough proof for her.
Food and Drug Administration officials have recently said certain psychedelic drugs show promise as potential treatments for a variety of disorders. Oregon and Colorado have already decriminalized magic mushrooms and other psychedelic drugs.
A UC Berkeley poll in 2023 found more than six in 10 Americans support legalizing regulated therapeutic access to psychedelics.
- San Francisco

When Kenny Choi jumped into the backseat, he never thought he would be introducing his ride share driver to National Public Radio. The hour-long ride to the airport turned into a conversation that included politics, the economic divide, and the cultural differences between the East Coast and the West Coast.
Featured Local Savings
More from cbs news.

Logan Webb extends scoreless streak to 19 innings as Giants beat Mets 5-1

Venerable San Francisco LGBTQ bar the Stud reopens at new location

Tyler, the Creator headlines Outside Lands 2024 with The Killers, Post Malone

Watch: Whale carcass that washed ashore in Alameda towed across San Francisco Bay
Kellogg School of Management at Northwestern University
Entrepreneurship Healthcare Policy Apr 19, 2024
Psychedelic-assisted therapy is going mainstream. how will the industry grow around it, while significant barriers remain—including regulatory uncertainty and the difficulty of scaling a labor-intensive treatment method—industry leaders see a path forward..
David Schonthal
Michael Cotton
David Esselman
In recent years, psychedelics have moved beyond their reputation as the mind-expanding substances that fueled countercultural explorations. Much of this surge of interest has to do with new discoveries about these drugs’ therapeutic potential.
Recent clinical trials suggest that MDMA, ketamine, and psilocybin, when taken under medical supervision, can treat a range disorders, including addiction, major depression, and PTSD. In 2017, MDMA (also known as ecstasy) was designated a “breakthrough” medication by the FDA. Last year, a study found that ketamine might be more effective than electroconvulsive therapy in treating major depression. Meanwhile, psilocybin has been shown to ease the anxiety of terminal cancer patients. Last year, Oregon legalized its use in regulated settings.
For proponents, this research demonstrates that psychedelic-assisted therapy (PAT) might have a role to play in addressing our mental health crisis. And as states move to legalize controlled use of these substances, an industry is taking shape, with some predicting a paradigm shift on par with the rise of SSRIs or medical cannabis.
“The public discourse around behavioral health has elevated in a way where this conversation can happen now,” says David Schonthal , a clinical professor of strategy and Director of Entrepreneurship Programs at the Kellogg School. “There is a recognized need for it. And there’s a growing interest from states and insurers who recognize the power of these medicines, not just in terms of their therapeutic benefit, but also in terms of their business impact.”
But what might this industry look like? There are still significant barriers, including regulatory uncertainty, the hesitance among major insurers to cover novel medicines, and the difficulty of scaling a labor-intensive treatment method. Not to mention the PR challenge of overcoming the cultural stigmas attached to these powerful compounds.
Kellogg Insight assembled a group of entrepreneurs, philanthropists, and investors in the psychedelic-assisted-therapy industry to discuss the way the field is developing, what’s holding it back, and what to expect from the future of psychedelics.
The long journey to acceptance
While attempts to bring PAT into the mainstream are not new—more than a thousand studies on psychedelics were launched in the 1950s and 60s—the drugs’ associations with the 60s counterculture led to regulatory backlash. In 1970, President Nixon had psychedelics classified as Schedule 1 controlled substances, effectively cutting off research on the drugs for decades.
In the late 1990s, however, the DEA opened the door to regulatory approval again. By 2019, Johns Hopkins had launched its Center for Psychedelic and Consciousness Research , a major step in legitimizing the field.
This turn toward psychedelics reflects a broader frustration many have with the mental-healthcare status quo.
“Behavioral-health science in the United States has not been particularly well cared for,” says Michael Cotton, an investor and philanthropist who has owned and operated Medicaid-managed care plans for twenty years. “In fact, we’ve seen a lot of disinvestment in the last few decades. A lot of people don’t have access to mental health services.”
The data on mental health in the U.S. is certainly bleak, with overdose and suicide rates skyrocketing over the past two decades, despite the widespread adoption of antidepressants and other medical treatments.
The hope is that PAT, which aims to address underlying conditions through a temporary shift in the patient’s consciousness, can induce the kind of emotional and cognitive experience that leads to lasting behavioral change. For advocates of PAT, this therapeutic model, in which the medicine and therapy are administered together, has advantages over SSRIs, whose longer-term efficacy is still unclear.
“Neuroplasticity is very real,” says David Esselman , senior advisor to BrainFutures , a nonprofit focused on bringing mental-health innovations, including psychedelic-assisted therapy, into healthcare systems. “These compounds allow you to incorporate insights you have in treatment into your life. This new class of drugs could be monumentally impactful, affecting tens of millions of people.”
The challenges of integrating PAT into the medical system
Despite its clinical promise, there is still the challenge of integrating PAT into existing treatment systems. Not everyone is keen to embrace a class of drugs more commonly seen at raves than in clinics. Even pioneers such as the late Dr. Roland Griffiths have said they worry about provoking another regulatory backlash by moving too quickly.
But Americans’ attitudes might be changing, especially through the adoption of psychedelics by groups not typically associated with the counterculture.
“We’re seeing resonance, particularly in more-conservative areas, around the mental-health needs of first responders and veterans,” Cotton says. In fact, U.S. veterans have been leading the lobbying effort. Women who suffer from PTSD as a result of sexual assault are also strong candidates for psychedelic treatments, as are patients struggling with addiction. Kentucky even considered putting some of its opioid settlement money toward research into psychedelic treatments for this latter group, though the plan eventually fell through.
“When you talk about these options and you show the possibilities, even those who are skeptical of psychedelic drugs see that when you take the drugs plus therapy, it’s monumentally more effective than either the drug or the therapy alone,” Esselman says. “And I think that when the FDA approves MDMA, there’s going to be a huge spike in interest.”
“The public discourse around behavioral health has elevated in a way where this conversation can happen now.” — David Schonthal
Still, it’s going to take more than agency approval for the industry to gain traction.
One major hurdle is the question of training and licensing for therapists. It’s not clear who would qualify to administer these drugs in a therapeutic setting or what the best practices should be. The University of Pennsylvania’s nursing program, together with Columbia’s school of social work, has begun to expand its curriculum to include training in psychedelic-assisted therapy to new nurses and social workers, but this program is still in its pilot stage. Meanwhile, those who know the drugs best tend to come from underground alternative-wellness backgrounds, making for a tricky integration into the traditional medical system.
Major insurers could represent an even larger stumbling block. “The large payers are going to be skeptical, and clinical trials won’t get them there,” Cotton says. “They want to see actual data. They want to know what to expect in terms of reducing hospital admissions or avoiding other services.”
What could push the treatment forward through traditional medical channels, however, is pressure from the business community. “There’s a growing recognition that the current mental-health crisis is now affecting our economics, our business environment, and our workforce,” says Esselman.
Indeed, Cotton says, some of the earliest proponents of psychedelic treatments are currently coming from “self-insured employer groups who emphasize the mental well-being of their employees. Some of them are already purchasing ketamine plans that are not offered by traditional insurance.”
What Oregon’s legalization shows
In Oregon, the first state to legalize psilocybin , an alternative model is taking shape—one that doesn’t rely on fully integrating psychedelic therapy into the medical system.
Instead, trained “facilitators”—licensed by the Oregon Health Authority—offer what the state refers to as “psilocybin services.” Patients don’t need a medical diagnosis to participate, and facilitator certificate programs—which require anywhere from three months to a year of coursework and practicum hours—are open to anyone with a high-school diploma who has passed a background check.
“Everyone expected it to be like cannabis, where there’d be a rush of people wanting to grow mushrooms,” says Ryan Reid , the founder of Bendable Therapy ‚ a nonprofit that educates and prepares potential therapy patients, and Drop Thesis , a for-profit company that includes psilocybin manufacturing and service centers. “But what actually happened was that everyone jumped in to become facilitators. By the end of this year, there might be over a thousand trained facilitators from fifteen or so different schools, but there are only about two dozen services centers licensed in the state right now. There are way more facilitators than there are service centers.”
In part, that’s because conservative county officials who oppose psychedelics have tried to make these centers economically unfeasible, as they did when the cannabis industry cropped up after legalization. “They learned how to throw enough wrenches into the works that you can’t start up,” he says.
But Reid says cannabis isn’t the best analogy for psilocybin services in Oregon, because cannabis is primarily about the sale of a product, where psilocybin is primarily about the sale of a service—facilitation—which is very labor-intensive.
When a typical PAT session—which includes preparation, dosage, and integration—is 12 hours one-on-one with a licensed professional, it’s hard to see how these service centers will be able to design their treatment systems to be sustainable. And once decriminalization expands, that may take a further bite out of the economic viability of PAT.
“I think you’ll probably end up with two-tiered market,” he says. “You’re going to have these little boutiques that offer psilocybin with a mental-health focus. And then you’ll have dispensaries for people who want the consciousness-expansion experience. There will always be demand for the mental-health-access approach, but it’s hard to keep viable.”
Cotton sees group therapy as a possible way forward. “Clinics will need to be embedded in the fabric of local communities,” he says. “Group models will be absolutely crucial, especially for lower-income communities.”
Schonthal points to Alcoholics Anonymous as an example of the power of group therapy. There’s also an interesting pharmacological wrinkle to the birth of AA. The group’s founder, Bill Wilson , credited the supervised use of the psychedelic LSD for his break with addiction.
“AA’s entire model is built upon this concept of having each other’s back. If you’re thinking about how to scale, creating a community is one way to do that.”
What’s next for psychedelics?
Whatever path the industry takes—prescriptions, dispensaries, community-based programs, or some combination of the above—there’s the question of who will benefit and who will be disrupted. The pharmaceutical industry, for example, might not welcome a shift away from Zoloft or Prozac.
“There’s no question the introduction of psychedelics upends their model,” Cotton says of the pharmaceutical industry, which has already been disrupted by patients’ increased access to cannabis.
And while psychedelic enthusiasts say their goal is to fill gaps in care created by years of disinvestment in mental-health services, it may be tough to find business models that will make a significant difference in the mental health of millions.
“Low-income, marginalized communities are where the bulk of trauma is happening. These are the communities that could benefit the most from transformational healing,” Cotton says. But finding profitable business models here is the most difficult to pull off, meaning governments and philanthropists may need to step in. “It’s going to take a lot of work to figure out how to get access to as many people as possible.”
Clinical Professor of Strategy; Director of Entrepreneurship Programs at Kellogg; Faculty Director of the Zell Fellows Program; Director of the Levy Institute for Entrepreneurial Practice
Andrew Warren is a writer based in Southern California.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Exercise cuts heart disease risk in part by lowering stress, study finds

How to realize immense promise of gene editing

Women rarely die from heart problems, right? Ask Paula.

Charles M. Stang (from left), Christine Hauskeller, Mason Marks, and Roman Palitsky.
Photos by Niles Singer/Harvard Staff Photographer
How to untangle ethics of psychedelics for therapeutic care
Experts from law, philosophy, spiritual care discuss issues surrounding research, safer use, kicking off Divinity School initiative
Samantha Laine Perfas
Harvard Staff Writer
There’s a telling paradox emerging in the world of treatment with psychedelics, according to Christine Hauskeller. In the past, doctors would be concerned if patients said they were hearing voices and seeing spirits. But now, it may be the doctors themselves who are responsible for those hallucinations.
“We use and induce states of what we called ‘madness’ before to cure what we’ve called ‘madness’ before and somehow create health,” said the philosopher with training in sociology and psychology at an April 16 discussion at Swartz Hall. “This is phenomenal.”
Hauskeller spoke at the first event of the Center for the Study of World Religions’ new psychedelics and ethics initiative, part of the University’s recently launched Study of Psychedelics in Society and Culture , which seeks to gather scholars and practitioners from different disciplines to discuss the tangle of issues surrounding clinical use of the drugs. In this inaugural session, speakers explored how approaches from law, philosophy, and spiritual care could help better inform ethical research and promote safer use.

“[We’re seeing] an explosion of interest and enthusiasm, but perhaps too little regulation — that’s open for debate — and a fast-moving landscape,” said Charles Stang , director of the Center for the Study of World Religions.
“Psychedelic experiences don’t match to psychedelic substances, in not only that the same dose of the same substance doesn’t induce the same effects in different people, or even in the same person twice.” Christine Hauskeller
Hauskeller said that in her view, there are two ways of approaching the study of psychedelics: by substance or experience. Studying the substance is straightforward: quantify dosages, test the chemical makeup, study the effects on different segments of the population. But studying the way patients experience the drug arguably matters more – and is a lot more complicated.
“Psychedelic experiences don’t match to psychedelic substances, in not only that the same dose of the same substance doesn’t induce the same effects in different people, or even in the same person twice,” said Hauskeller.
Bioethics provides a model for studying ethical questions around research on use. The pillars include promoting the good of society, avoiding harm to patients, and ensuring informed consent, along with fair access and distribution, she said.
These goals should be kept in mind as the medicalization of psychedelics increases, mass production looms, and financial incentives compete with ethical obligations. Hauskeller cited an example: how to keep treatment financially accessible. One session with psilocybin hallucinogenic mushrooms may cost $2,000, even though “these mushrooms grow basically everywhere.”
Mason Marks, a visiting professor at Harvard Law School from Florida State University College of Law, teaches a course on psychedelic law. He noted many parts of the legal landscape of using the drugs are largely “uncharted territory,” and informed consent is one area that needs improvement.

He found that even in clinical trials, only a small percentage of studies included informed consent as part of their process, which protects patients by equipping them with the knowledge of potential benefits and risks as well as informing them of other options if they choose to forego participation.
“We believe that people should fully understand what they’re getting themselves into.” Mason Marks
“We believe that people should fully understand what they’re getting themselves into,” said Marks, who is also the senior fellow and project lead of the Project on Psychedelics Law and Regulation at the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics.
In many ways, informed consent on psychedelics can follow best practices of other treatments. But psychedelic therapies also present problems that are unique: Adverse effects are often unknown. The prevalence and intensity of certain risks — prolonged side effects, permanent changes to perception, personality changes, altered metaphysical beliefs — require further research, he said.
Practitioners should be transparent about the risks and potential experiences associated with these treatments, with the goal of limiting patient exploitation or abuse, Marks said.

“In psychedelics, we often talk about these mystical-type experiences as a transformational, transient experience that impart some deep sense of knowledge and having made contact with something real.” Roman Palitsky
Roman Palitsky, an assistant professor and the director of Research Projects in Spiritual Health at Emory University, took a different approach to the ethics of psychedelic treatment. He suggested that using a SERT-based framework — spiritual, existential, religious, theological — would include the kinds of experiences that tend to arise from these treatments.
“In psychedelics, we often talk about these mystical-type experiences as a transformational, transient experience that impart some deep sense of knowledge and having made contact with something real,” Palitsky said. A SERT framework could include considering the religious or existential beliefs that patients have and how those beliefs overlap with their mental health concerns.
Palitsky mentioned that there are care providers already trained in integrated care: chaplains. They can add a lot to the conversations around incorporating SERT training into psychedelic care, which has a lot of potential to benefit the patient in enormous ways.
“As a colleague of mine once said, we’re not adding religion here,” he said. “We’re just not taking it out.”
Share this article
You might like.
Benefits nearly double for people with depression

Nobel-winning CRISPR pioneer says approval of revolutionary sickle-cell therapy shows need for more efficient, less expensive process

New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.
Good genes are nice, but joy is better
Harvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier
Ketamine bros are giving psychedelics a bad rap. That's a problem for those who need them.
These drugs could transform how we treat depression and other mental health ailments. let's not let the behavior of a small set of irresponsible users take that away from them..
In my work as a shaman, I once had the opportunity to help a woman who, barely into her 50s, was facing a painful death from bone cancer. Emaciated, her body wracked with pain, she told me she could not lie down in bed for fear of never getting back up. I accompanied her as she took a dose of psilocybin , a psychedelic compound found in magic mushrooms .
Over the next five hours, she went on a profound journey, one that allowed her to accept the fact of her imminent death and locate meaning in her experience. Afterward, she found that all the physical pain she had been experiencing had left her. “Now I believe in magic,” her husband told me. She lived her final few days in peace.
Years later, at a Miami dinner party hosted by a friend, I sat next to a woman who, after a short trip to the bathroom, returned and began laughing for no reason. She couldn’t string two sentences together. When I asked if anything was wrong, she said, “I’m so high on K ( ketamine ) right now, I can’t even think straight.”
Such is the confused state of psychedelics today.
I’ve seen firsthand both the transformative effects of psychedelics in treating mental health disorders as well as their casual abuse by people who think of them as a party drug.
I’ve become unnerved by this ketamine bro culture, which threatens to halt the exciting progress in psychedelic research over the past few decades.
Psychedelics are finally being taken seriously in medicine and therapy
Psychedelics herald a paradigm shift in the treatment of mood disorders. I’ve witnessed this as a trained and practicing shaman, providing personal guidance to hundreds of people – from cancer patients to veterans with post-traumatic stress disorder to people experiencing depression – as they come to terms with past instances of trauma or imminent death.
Becoming a shaman was the culmination of a circuitous journey to discover who I was and where I belonged. Raised in a confusing mixture of Judaism and Catholicism, I explored by apprenticing with teachers in a wide variety of faiths and traditions. I eventually found a home in the Santo Daime tradition, under the tutelage of Baixinha in Brazil, which is known for its syncretic religion that utilizes ayahuasca .
Through my training there, I saw the transformative effects of psychedelics when taken in a safe, controlled, therapeutic setting. (Ayahuasca is legal in Brazil .)
Countless studies over the past decade have highlighted the positive impact of substances like ketamine, psilocybin and other psychedelics.
Psilocybin, for instance, has demonstrated efficacy in treating conditions such as depression and anxiety. A 2016 study found that just a dose of psilocybin led to substantial, sustained reductions in depression and anxiety symptoms among cancer patients. Ketamine, traditionally used in medical settings as a short-term anesthetic, was suggested to have a “ robust and rapid effect on depression ” by a 2019 study.
These clinical and empirical data have been so encouraging that research is being conducted on psychedelics’ ability to alleviate symptoms of PTSD , anorexia and alcoholism .
It’s no secret the medical community has reached a tipping point: While we are tantalizingly close to a series of breakthroughs that together could revolutionize behavioral health treatment, we’re also a couple of bad trips away from stopping this research in its tracks.
The unique value psychedelics offer to behavioral health treatments is that they induce deeper states of consciousness, which allows for the accelerated healing of trauma. They also may promote neuroplasticity, the process by which the neural networks in the brain evolve and change.
Is it dangerous to smoke weed? What you need to know about using marijuana.
Rise of ketamine bro culture in Silicon Valley
Of course, rewiring the brain is a delicate process. It requires humility, trust, a controlled environment and an experienced guide. That’s why psychedelics’ newfound popularity as a party drug among the Silicon Valley elite is cause for concern.
The rise of ketamine bro culture not only trivializes the incredible therapeutic potential of psychedelics, it also could lead to a public backlash that jeopardizes the medical community’s freedom to further explore the lifesaving potential of these drugs.
Perhaps the poster child for this movement has been Elon Musk. His recreational use of LSD and mushrooms, among other illicit drugs, has been reported on in The Wall Street Journal, and he has publicly endorsed the benefits of ketamine, both in microdoses for his depression and full doses for fun.
Because Musk epitomizes the tech alpha male, it sends a concerning message about what psychedelics are all about. Silicon Valley leaders trumpet ketamine, shrooms and LSD as nonaddictive drugs that can disrupt one’s own habitual thinking, leading to new heights of inspiration both in the boardroom and after hours. Almost certainly, they’re taking them without the guidance of a professional.
What is ketamine? Elon Musk discusses using the drug in interview with Don Lemon
It’s certainly true that psychedelics can help achieve these altered mental states. But they can also lead to severe consequences if used in this haphazard way.
Just look around Silicon Valley and you can quickly see the consequences of psychedelic abuse. Zappos founder Tony Hsieh struggled with a ketamine addiction in the years before his drug-related death in 2020. Cash App founder Bob Lee died of stab wounds in 2023; his autopsy revealed evidence of alcohol, cocaine and ketamine consumption.
"Saturday Night Live" alum Pete Davidson entered rehab last year after taking ketamine daily for four years, not long before "Friends" star Matthew Perry died of “ acute effects of ketamine .”
Psychedelics stigma starting to wane. Misuse shouldn't stop progress.
It’s difficult to find reliable population-wide data on psychedelic abuse. That’s because they haven’t been widely used until recently and aren’t generally regarded as having potential for addiction.
One indicator, though, comes from a recent study finding that hallucinogen-associated visits to the emergency room in California jumped 54% between 2016 and 2022, from just more than 2,200 visits to nearly 3,500 visits. Ketamine is of particular concern, given the rise in its use in recent years.
The history of MDMA in the United States serves as a warning. Lauded in the 1970s for its therapeutic benefits – psychiatrists believed it enhanced communication during patient sessions – MDMA, or ecstasy, as it has come to be known, was quickly absorbed into rave culture.
This led to the Drug Enforcement Administration declaring in 1985 an “emergency ban” on MDMA, placing it on its list of Schedule I drugs: substances with no currently accepted medical use. (After far too long, MDMA is under priority review by the FDA Food and Drug Administration for use in treating PTSD. A decision is expected in August.)
So while we must be mindful of the hazards of psychedelic abuse, we also must be careful not to only regard them as a public health threat – lest we lose sight of their promising benefits.
To remedy this, recreational users must acknowledge their responsibility to society. Being visibly zonked out in social situations only adds to the narrative that psychedelics are simply a fun toy. And if you’re in a position of power, the responsibility is even greater. Trivializing the effects of these drugs could encourage people to take them outside of therapeutic settings.
As for the news media, it’s important that reporting is not overly focused on misuse. Journalists must take a balanced approach, remembering to highlight psychedelics’ therapeutic applications as much as their harmful ones. Failing to provide adequate context perpetuates misconceptions that we can’t afford.
The good news is that the stigma around psychedelics has begun to diminish with each new study. As their potential to revolutionize behavioral health therapy becomes increasingly evident, countless people grappling with debilitating physical, mental and spiritual pain are feeling hope.
Let’s not let the behavior of a small set of irresponsible users take that away from them.
Sylvia Benito is a family office portfolio manager and practicing shaman, and serves on the board of Beckley Retreats, one of the world’s first legal psychedelic retreat companies. She works with clients in jurisdictions where psilocybin is legal.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH

TECHNICAL NOTE: Our Glenwood/Silver City, New Mexico, transmitter at 92.1 FM is off air. Our engineers are diagnosing the problem. Thank you for your patience.
Analysis: patient-therapist bond may be key to treating depression with 'magic mushrooms'.
- 20240423b.mp3
Arizona’s advisory council on psilocybin research is soon expected to release a draft report about psychedelic-assisted therapy.
Researchers at Ohio State University say a provider-patient bond may matter most when treating depression with psychedelic mushrooms.
Ohio State researchers analyzed data gathered from a 2021 clinical trial that found psilocybin combined with therapy was effective at treating depression.
They concluded that the stronger the relationship between participant and therapist, the lower the participant’s depression score was one year later.
Arizona lawmakers set aside $5 million last year to study if psychedelic mushrooms can help people with pain, addiction and PTSD.
Research grants have been approved. But the money is unlikely to be spent before July, when the state can claw it back.
KJZZ is on Instagram!


IMAGES
VIDEO
COMMENTS
Field Trip Health uses evidence-based, legal psychedelic therapies that help you heal mental health conditions like anxiety and depression. For US Patients: ... Our holistic, hybrid journey blends ketamine, therapy, meditation, and wellness support in a flexible program that you can complete in-clinic or from the comfort of your home. ...
Get Matched with a Trusted Psychedelic Therapy Provider Near You. Hi there! We sincerely hope that you've found valuable takeaways that resonate with your current intentions. ... Preparation for a psychedelic trip is crucial to ensure a safe and meaningful experience. It involves several key aspects, such as setting intentions, creating a ...
A psychedelic guide differs from a trip sitter in that they'll take a more active role in guiding the psychedelic experience, whereas the main focus of a trip sitter is harm reduction. Both should be trained in harm reduction principles and know how to minimize fear and anxiety. Most importantly, they'll be present throughout the entire ...
For Tripsitters, Therapists, and Guides: Tips & Resources. Practice supporting others on their journeys. Spiritually mature, heart-centered psychedelic guides are gems for humanity. Here are some tips and resources for those seeking to grow in the work and serve as witnesses, mentors, and allies for other people's spiritual / psychedelic journeys.
Psychable.com is an online platform dedicated to connecting individuals with professional and trusted psychedelic therapists, clinics, and wellness practitioners. We offer resources, information, and a community for those interested in exploring psychedelic-assisted therapy and holistic mental health solutions.
Set the Stage for a Meaningful Journey. Intention-setting is a key part of the psychological ' set' —intentions set before a trip prime your mind to have related realizations. Your intentions provide focus and structure to the expanded state of consciousness induced by psychedelics [2]. Feeling comfortable in your physical and social ...
A psychedelic trip is all of these things, and your experience will be determined by how you prepare for it. There are two steps: being capable and arranging your resources. ... Psychedelic preparation is like therapy without the therapist. There may be therapists in the future, but today's therapists can't help you.
What to do. The most effective way to minimise the risk of a bad trip occurring is to prepare well. The Johns Hopkins advice is for guides and therapists to discuss the broad range of psychological effects that can be experienced under the influence of a psychedelic, including out-of-body sensations, the evocation of powerful memories, distortions to time and space, and feelings of oneness ...
Administering psychedelic-assisted therapy is vastly different for professionals used to conventional mental-health treatments, says Bit Yaden, a psychiatrist at Johns Hopkins Medicine, who is ...
In psychedelic-assisted therapy this is called integration, and it involves talk therapy, journaling, and goal-setting. "There's actual work involved," Levy says.
Therapists undergo several years of training and practice before they receive licensure. Since the material that arises in a psychedelic trip can be incredibly personal, complex, and is often related to past trauma, doing integration work with a licensed therapist can facilitate the healing process.
2. Clinical trials are your only legal option for most psychedelics. One of the safest ways to try psychedelic-assisted therapy—whether you're exploring MDMA, psilocybin, LSD, or other ...
Psychedelic therapy shows promise for the treatment of conditions such as anxiety, depression, and addiction. Learn about current research on its use. ... The use of psychedelics can also result in what is known as a "bad trip." These experiences are marked by intense and terrifying feelings of anxiety and the fear of losing control.
Enosis Therapeutics is developing virtual reality technology for psychedelic-assisted therapy. Credit: Enosis Therapeutics. When someone embarks on a psychedelic trip, they have little control ...
Key Principles of Psychedelic Integration Therapy. Non-judgmental Space: Integration therapy provides a safe and non-judgmental space for individuals to share their psychedelic experiences openly. ... Similarly, a psychedelic trip could also spur up feelings of existentialism and spirituality that may need to be integrated. Perhaps a person is ...
A therapeutic approach to psychedelic usage, or specifically psilocybin-assisted therapy, involves medicinally using psilocybin or other psychedelic substances for therapeutic benefits with a guide. Psychedelic facilitators or guides provide general support during a trip as well as support around preparation and integration and tips, tools, and ...
The study, which analyzed a 2021 clinical study involving 24 patients using psilocybin-assisted therapy to treat severe depression, found that participants with stronger self-reported connections ...
Psychedelic therapy is on its way to becoming a mainstream medical treatment in mental health care. In 2020 and 2022, residents of Oregon and Colorado voted to legalize the use of psilocybin, the ...
A psychedelic trip on magic mushrooms led me to embrace my neurodiversity, and now, I help others do the same as a psychedelic-assisted therapy facilitator. Twelve years ago, I embarked on a transformative psychedelics journey that opened my eyes to my true self. I did not know then that this trip into my subconscious would completely change my ...
Many consider music to be core to the psychedelic experience. Going back millennia, music features prominently in the indigenous use of psychedelics (such as the rattle and drum used in peyote ceremonies and the icaros, or traditional indigenous Amazonian songs, performed in ayahuasca ceremonies).In a Western context, by the late 1950s, music's important contribution to psychedelic therapy ...
Drug effects have dominated the national conversation about psychedelics for medical treatment, but a new study suggests that when it comes to reducing depression with psychedelic-assisted therapy, what matters most is a strong relationship between the therapist and study participant. Researchers analyzed data from a 2021 clinical trial that fou...
Psychedelics Today: Updates from MAPS: Current Initiatives, Psychedelic Science 2025, and Music as a Bridge In this episode, Joe interviews Devon Phillips: Community & Partnerships officer for the Multidisciplinary Association for Psychedelic Studies (MAPS).
By Kenny Choi. April 17, 2024 / 7:31 PM PDT / CBS San Francisco. The push to legalize psychedelic-assisted therapy treatments continues, as patients say it helps and the FDA recently said some ...
The University of Pennsylvania's nursing program, together with Columbia's school of social work, has begun to expand its curriculum to include training in psychedelic-assisted therapy to new nurses and social workers, but this program is still in its pilot stage. Meanwhile, those who know the drugs best tend to come from underground ...
Ohio State University. Levin, A. W., et al. (2024) The therapeutic alliance between study participants and intervention facilitators is associated with acute effects and clinical outcomes in a ...
Christine Hauskeller. Hauskeller said that in her view, there are two ways of approaching the study of psychedelics: by substance or experience. Studying the substance is straightforward: quantify dosages, test the chemical makeup, study the effects on different segments of the population. But studying the way patients experience the drug ...
The suite of benefits your company offers may one day look like this: vision, dental, 401 (k) match and psychedelic-assisted therapy for mental health. A small but growing number of companies are ...
Countless studies over the past decade have highlighted the positive impact of substances like ketamine, psilocybin and other psychedelics. Psilocybin, for instance, has demonstrated efficacy in ...
In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called "bad trip"—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may ...
Arizona's advisory council on psilocybin research is soon expected to release a draft report about psychedelic-assisted therapy. Researchers at Ohio State University say a provider-patient bond may matter most when treating depression with psychedelic mushrooms.. Ohio State researchers analyzed data gathered from a 2021 clinical trial that found psilocybin combined with therapy was effective ...